
A YEAR OF GROWTH

Message from the chair

Joy Lincoln, PhD, Peter Sommerhauser Endowed Chair
for Cardiac Quality, Outcomes and Research, Children’s Wisconsin
A Chinese proverb states, "Be not afraid of growing slowly; be afraid only of standing still.” Even as a young child I wanted to start tomorrow before the day had ended, despite knowing that perseverance may be the defining trait needed for building a strong foundation for success.
2022 has been another extraordinary year of growth for the Herma Heart Institute’s (HHI) Quality, Outcomes and Research (QOR) Program. We have expanded our research team by more than 40 percent and increased our active research awards by 14 percent.
This includes new funding from Advancing a Healthier Wisconsin (Aoy Tomita-Mitchell, PhD; Kasey Chaszczewski, MD), the Greater Milwaukee Foundation (Sal Ginde, MD), Additional Ventures (Andrew Spearman, MD), Herma Heart Institute Innovation Funds (Joy Lincoln, PhD; Andrew Kim, MD, PhD; John Baker, PhD; Michael Mitchell, MD; Jake Schott, MD), the Michael H. Keelan, Jr. Scholar Award (Lu Han, PhD), and the National Institutes of Health (NIH) (Joy Lincoln, PhD; Andrew Spearman, MD; Margaret Samyn, MD; Janette Strasburger, MD).
Notable funding award recipients include faculty teams within basic, translational and clinical science disciplines. Dr. Spearman received the HHI’s first NIH Career Development Award (K08) for work delineating the mechanisms underlying adverse blood vessel formation in single ventricle patients. We have leveraged our funding opportunities to support the training and professional growth of the next generation of physician-scientists, including undergraduates, medical students, graduate students, pediatric residents, clinical and post-doctoral fellows, as well as early career investigators.
In addition to comprehensive cardiac care, HHI pioneers solutions supporting “whole child” needs through clinical outcomes for kids born with congenital heart disease. In 2022, the Educational Achievement Partnership Program, led by Kyle Landry, MEd, and Cheryl Brosig Soto, PhD, expanded from focusing on advancing long-term educational achievements of children only with cardiac care needs to patients receiving care for chronic illness in other pediatric clinics, including oncology, complex care, neuropsychology and asthma. Salil Ginde, MD, and Benjamin Goot, MD, received funding from the Greater Milwaukee Foundation to determine socioeconomic differences in risk for cardiovascular disease in kids in southeast Wisconsin. This work compliments endeavors, led by Nikki Singh, MD, in identifying socioeconomic risk factors in pediatric cardiac transplant recipients.
As we build upon our foundation in the years ahead, HHI will continue to strengthen existing programs, while creating new collaborations with our local and national partners. Plans are underway to nationally expand the clinical application of our existing Cord Blood Program. Patient families pre-diagnosed with congenital heart disease in utero will bank umbilical cord material under clinical-grade conditions at no cost, with the intent of utilizing the patient’s autologous cells to generate surgical material for reconstructive cardiac repair.
The COVID-19 pandemic has shifted how we interact, care
for our patients and advance research and discovery. It has
also taught us to stay strong, work together and determine to be our best in caring for the sickest kids with congenital heart disease and their families.
Joy Lincoln, PhD
Peter Sommerhauser Endowed Chair for Cardiac Quality, Outcomes and Research, Children’s Wisconsin
Director of Cardiovascular Research, Herma Heart Institute Professor and Associate Section Chief, Pediatric Cardiology, Medical College of Wisconsin




George Hoffman, MD
George Hoffman, MD
Pioneer, friend, mentor
Remembering James S. Tweddell, MD
Lifesaving heart surgeon James S. Tweddell, MD, passed away in 2022, at the age of 62 after a battle with cancer. He had a considerable impact on the children, both in the Herma Heart Institute and around the world, during his 20 years of service at Children’s Wisconsin.
Michael Mitchell, MD, medical director of cardiothoracic surgery at Children’s Wisconsin and surgical director of the Herma Heart Institute, spent nearly a decade working with Dr. Tweddell as a colleague.
“I was aware of his progress and development at the program from the time I was in medical school back in 1993,” he said. Dr. Mitchell joined Children’s Wisconsin in 2006, but he’d been paying close attention to Dr. Tweddell’s and the heart team’s work all along.
“He and the team here did phenomenal work on developing treatment for patients with hypoplastic left heart syndrome,” said Dr. Mitchell. “They drove the development of the program, which was achieving some of the best outcomes for the treatment of this lesion — better than many other centers around the country. That was a very exciting time for the program, and it really led to significant programmatic development.”
Dr. Mitchell added that beyond being a pioneer in surgical treatment, Dr. Tweddell was a strong champion for the team approach to patient care. “He had an approach that involves the surgeons working with the cardiologists, the anesthesia team, advanced practice providers and ICU nursing staff, all together as part of a team to generate the best outcomes for patients with congenital heart disease,” he said.
In addition to his talent as a heart surgeon, Dr. Tweddell was known and loved for his skill on the banjo, which he regularly shared on air
during the annual Children’s Wisconsin Miracle Marathon radiothon.
“He was an excellent mentor and friend,” said Dr. Mitchell. His patients and colleagues, with whom he built strong bonds and lasting relationships, will miss him dearly.
Carrying on the Legacy
In honor of Dr. Tweddell’s lifelong commitment to advancements in cardiac care, the James S. Tweddell Chair in Clinical Cardiac Research has been established at Children’s Wisconsin. If you are interested in contributing to this endowed chair, contact the Children’s Wisconsin Foundation at foundation@childrenswi.org.
The first person to hold this position is George Hoffman, MD, anesthesiologist-in-chief, medical director of Pediatric Anesthesiology and associate medical director of Pediatric Critical Care, and chief and professor of Pediatric Anesthesiology at the Medical College of Wisconsin.
Innovation Fund Awards
The Herma Heart Institute Innovation Fund was created in 2018, to explicitly support research, quality improvement and innovations in cardiovascular related education and training. This year, a total of four grants were awarded for research pilot studies, quality improvement projects and a collaborative programmatic award.
The 2022 Innovation Fund Award winners
HERMA HEART INSTITUTE RESEARCH GRANTS
Generating heart valve cell populations from human
umbilical cord blood — Joy Lincoln, PhD
- The HHI has an active cord blood bank that stores umbilical material collected from patients with congenital heart disease in a clinical grade facility. This pilot award is isolating endothelial progenitor cells from umbilical blood and effectively differentiating them toward functional valve endothelial cells and valve interstitial cells that phenotypically mimic the native valve. Successful completion will provide the field with autologous
cells that recapitulate native valve cell populations that can be used to develop biocompatible tissue for engineered heart valves to improve the outcome of kids with heart disease in the future.
Head-to-head comparison of mitochondrial cell-free DNA and cardiac troponin as a biomarker for the extent of cardiac injury following high-risk infant cardiac surgery — Michael Mitchell, MD;
Jake Scott, MD
- Dr. Mitchell and Dr. Scott are working on ways to quantify injuries that occur during cardiac surgery with the goal of reducing those injuries to improve patient outcomes. “We are studying something called cell-free DNA in the patients that we operate on, as both a marker of inflammation, and also a part of inflammation in patients who’ve had open heart surgery,” Dr. Mitchell said.
HERMA HEART INSTITUTE QUALITY IMPROVEMENT GRANTS
School Screening and Health Plan Improvement Project — Kyle Landry, MEd; Christie Reuhl, JD, MBA
- Children with heart disease are at risk for an array of deficits that may affect development, psychosocial skills, and academic attainment. Previous studies have found school staff are not trained to recognize heart-brain-body connections, and this knowledge and information gap may lead schools to inadvertently not qualify the child for access to support services. The Educational Achievement Partnership Program (EAPP) is a hospital-based service that collaborates with multidisciplinary health, educational and community care teams to implement medically informed interventions in school settings. Globally, the School Screening and Health Plan Improvement Project aims to improve screening for school concerns and access to EAPP services and hospital-based school health plans recommendations for school-aged cardiac patients at the Herma Heart Institute at Children’s Wisconsin
HERMA HEART INSTITUTE PROGRAMMATIC GRANTS
Herma Heart Institute Tissue Repository — Precision Medicine Program
- The Precision Medicine Program has an active bank of discarded tissue, blood or cell samples donated at the time of birth or during corrective surgery from patients diagnosed with congenital heart disease. Research and clinical studies are focused on utilizing patient cells to develop surgical material that can be implanted back into the child to fix congenital structural malformations of the heart in the future.



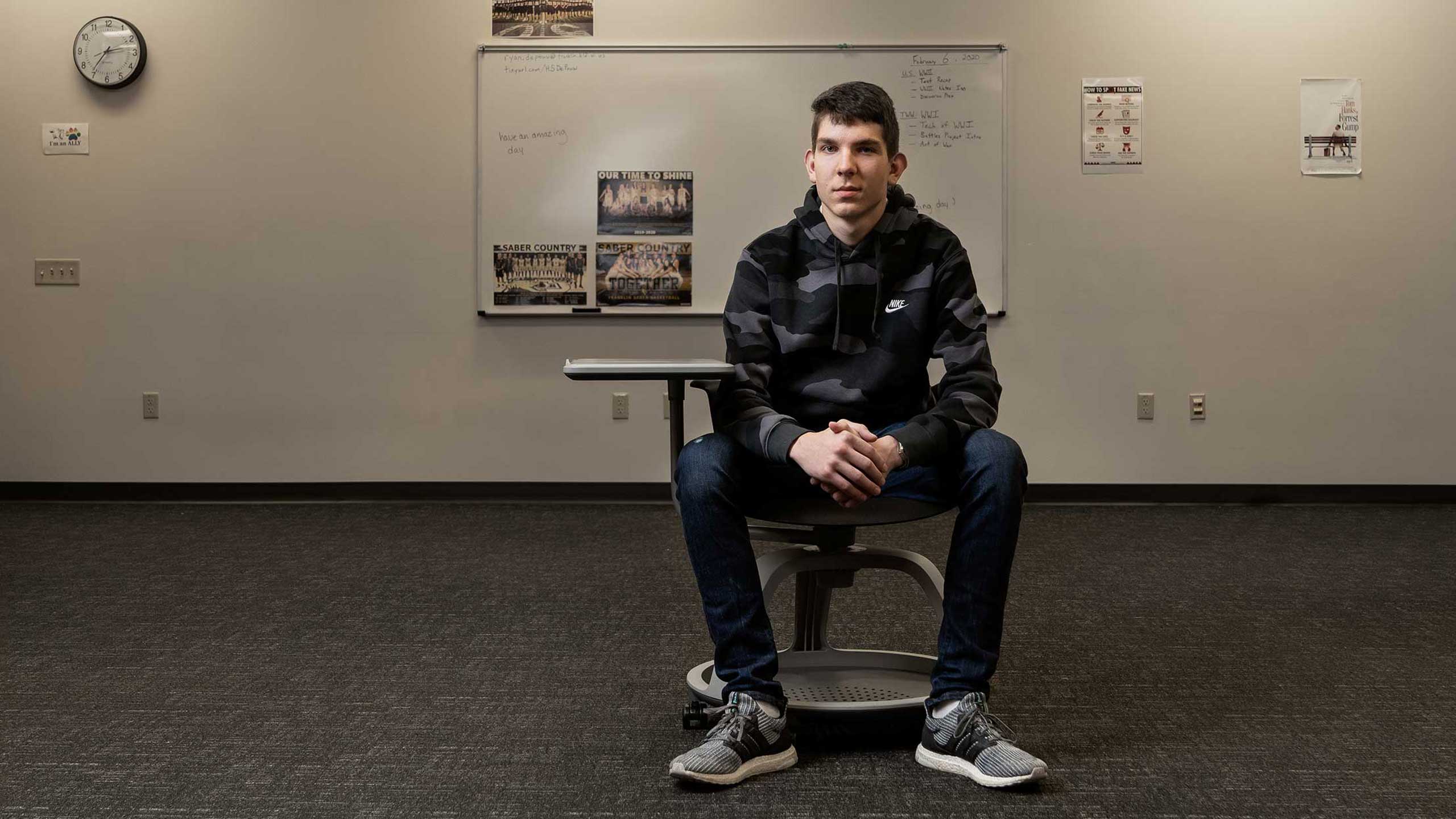
Home-grown program brings life-saving training to schools across the nation
More than 200. That’s how many lives have been saved since Project ADAM began in 1999. Run by the Herma Heart Institute (HHI) at Children’s Wisconsin, Project ADAM provides programming and resources to ensure the availability of automated external defibrillators (AEDs) and CPR training in schools. The program bears the name of Adam Lemel, a 17-year-old Whitefish Bay high school student who died from sudden cardiac arrest while playing basketball. An AED could have saved him.
MAKING A DIFFERENCE
The initial efforts of Project ADAM centered on education about sudden cardiac arrest, especially in children, and encouraged schools to have AEDs available. But it soon became clear that just having AEDs in the building didn’t ensure an appropriate response during a cardiac emergency. So, in 2016, Project ADAM initiated the Heart Safe School (HSS) Program in Wisconsin.
The program is built around 14 components based on best practices in school-based cardiac emergency preparedness. It is designed to allow for an ongoing partnership between the school program and the hospital. Initially, HHI, which still manages Project ADAM, focused on schools in the state, spreading the word through workshops, consultations, school nurses, volunteers and HHI’s Educational Achievement Partnership Program, which advances long-term educational achievement in children with chronic illness through collaboration, knowledge, advocacy and commitment.
An HHI study of the program recently presented at the 2022 Children’s Hospital of Philadelphia Cardiology meeting found that, within three years, 436 Wisconsin schools applied for HSS designation. Of those, 177 already had a comprehensive HSS program in place and were immediately awarded the designation. Of the remaining 259, 139 (54 percent) achieved HSS designation within four years, with a median time from entry to completion of 335 days. The study found that the most challenging aspect of HSS designation was allocating staff time for training, while the most useful resources were customizable templates and the HSS checklist.
GROWING THE PROGRAM
Soon after the program launched in Wisconsin, other institutions wanted to emulate it. The first affiliate was Children’s Healthcare of Atlanta. Project ADAM administrator Alli Thompson began talking about the HSS program at conferences she attended and with other colleagues around the country, who wanted to know how they could be part of the program. Today, there are 38 affiliate programs in 29 states and more than 4,129 Heart Safe Schools across the nation. Affiliates offer free school consultations, templates and videos that enable schools to earn their HSS designation.
“Most sites interested in doing similar work want to do it because they’ve lost somebody in their community, and they know it’s preventable,” said Thompson. “They want to wrap it in as part of their cardiology programs to say they’re protecting the community in the schools.”
Some of the fastest growth came during the pandemic, with 15 new affiliate programs added since mid-2019. “It’s a little surprising that people were advocating and pushing within their own systems during a time when it was hard to ask for extra things in health care, but that demonstrates the importance of this work,” said Thompson.
The Children’s Wisconsin affiliate also saw tremendous growth during the pandemic, adding 13 counties and 130 schools throughout the state. “The national growth has been exponential,” said Anoop Singh, MD, medical director of Project ADAM. “We’ve gone from hoping people would be interested in it to saying this has just taken off. It’s very exciting to get to the point where it’s really caught fire.”
LOOKING AHEAD
The Project ADAM team is not sitting back and resting on their past success. “There’s still a lot of education that needs to happen,” said Thompson. They aim to acquire affiliates in all 50 states and expand the revenue stream beyond its current funder, the Children’s Wisconsin Foundation.
Project ADAM is expanding its reach beyond schools through its new Heart Safe Youth Sports & Community Sites initiatives. The goal is to ensure that athletes, coaches, referees and spectators at community sports complexes and youth sports programs have access to AEDs, people trained in CPR/AED and a practiced plan.
“The Heart Safe Youth Sports & Community Site initiative is a natural expansion of what we were already doing,” said Dr. Singh. As with the HSS initiative, the new program is starting locally with two Wisconsin athletic facilities and three youth sports teams.
According to Thompson, they’ve discovered that working with outdoor sports programs run by volunteer coaches requires a different approach than working with schools. “We’re approaching it from a ‘medical time out,’ perspective,” she said. That means training the coaches in general CPR skills and teaching them to take a brief “time out” before every game to know where the nearest AED equipment is.
Another major effort is advocacy. For instance, Project ADAM was a strong supporter of the requirement that all Wisconsin high schoolers receive CPR and AED instruction before graduating. “The idea is that there are certain skills that are public health life skills,” said Dr. Singh. “This creates an army of adults who can respond to emergencies.”
Project ADAM’s expanding scope won’t distract from the program’s primary mission: Guiding schools in obtaining AEDs and training staff on how to use them so they can become an HSS. “We want people to know that this is a really great standard to have,” said Thompson.



Lab spotlights

Spotlight on Andrew Spearman, MD
Spotlight on Andrew Spearman, MD
Getting real data
A $750,000, five-year National Institutes of Health (NIH) K08 grant breathed new life into the research of Andrew Spearman, MD, a pediatric cardiologist at Children’s Wisconsin and assistant professor of Pediatric Cardiology at the Medical College of Wisconsin. His work focuses on changes in pulmonary circulation, including the development of pulmonary arteriovenous malformations (PAVMs) or abnormal connections between the arteries and veins in the lungs that occur in children with hypoplastic left heart syndrome.
This congenital disease, in which the left side of the heart is underdeveloped, requires numerous surgeries. Dr. Spearman and his team are trying to figure out why these children later develop PAVMs, which can cause hypoxia (low oxygen levels), dramatically impacting quality of life. To do that, they are studying the genes and proteins responsible for the remodeling.
The NIH grant is a career development grant that allows
researchers like Dr. Spearman to develop new skills for basic and translational research. It also protects 75 percent of his clinical time for research.
“That gives me protected time to develop additional skills that will allow us to study these pulmonary AVMs in a couple of different ways with new and advanced techniques,” he said.
That includes studying PAVMs in vitro in the lab, and in vivo in an animal model. “In vivo lets us overcome obstacles that a petri dish just can’t do,” he said.
For example, preliminary data from the lab identified higher-than-expected levels of certain proteins leaving the liver, suggesting it might play a key part of the PAVM disease process. So, Dr. Spearman’s team knocked out the gene for the potential “hepatic factor” in mice to see if their hypothesis was correct.
“Nothing happened,” he said. But while the outcome was unexpected, the finding was important: Hepatocytes don’t express their candidate protein even though levels are high in the hepatic vein. They published the results in the journal Frontiers in Cardiovascular Medicine.1
“It shows that, despite our very strong clinical observations, we don’t have real experimental data that helped us pinpoint anything,” he said.
And to advance in science you need data. The findings convinced Dr. Spearman to shift from a genetic mouse model to a surgical animal model to get a better idea of what’s driving the disease process. “Then we can identify data-driven targets and work backward to a genetically engineered animal model,” he said.
Without this basic research, it will likely be impossible to figure out why these kids get PAVMs. “Most people who get these NIH awards in pediatric cardiology are clinically focused,” said Dr. Spearman. “We just don’t have a lot of basic science translational research focused on problems in our field. We definitely need to grow that aspect of research.”
1 Merbach M, Ramchandran R, Spearman AD. Hepatic factor may not originate from hepatocytes. Front Cardiovasc Med. 2022;9:999315.


Spotlight on Margaret Samyn, MD
Spotlight on Margaret Samyn, MD
Exploring new approaches
Margaret Samyn, MD, MBA, a pediatric cardiologist at Children’s Wisconsin and professor of Pediatric Cardiology at the Medical College of Wisconsin, has recently garnered her first funding from the National Institutes of Health (NIH) by partnering with investigators at Vanderbilt University (Jonathan Soslow, MD, MSCI) and Carle Foundation Hospital (Bruce Damon, PhD) to write a multi-principal investigator grant focused on characterizing pediatric heart transplant recipients by cardiac magnetic resonance imaging (MRI).
Dr. Samyn’s career has been unique in many ways, as she was a community pediatrician before completing a pediatric cardiology fellowship and serving as clinical research director at two fortune 500 pharmaceutical companies. She returned to academic clinical cardiology in 2003, and has 18 years of expertise in cardiac MRI. Dr. Samyn’s past experience in running multicenter clinical pharmaceutical trials makes her well-suited to co-direct this NIH-funded research.
The five-year, $3.3 million grant will enable a multicenter study to see if MRI can predict acute rejection in pediatric heart transplant patients. Currently, rejection is identified primarily through biopsy, which is invasive, expensive and carries its own risks.
Sampling error is another issue with heart biopsy, because the biopsy catheter can only reach tissue on the right ventricular (RV) side of the interventricular septum.
“Rejection is a heterogeneous process and may affect the heart in a patchy fashion. Acquiring samples from the RV septal surface may miss affected regions, if this part of the heart is not inflamed. The interventionalist might select tissue from a region that has previously been biopsied, so the sample may show scar rather than an acute process. This also creates sampling error,” Dr. Samyn said.
The genesis for Dr. Samyn’s NIH grant came from her attendance at the Society for Cardiovascular Magnetic Resonance (SCMR) annual meeting years ago. She listened to a session on the use of cardiac MRI for adult heart transplant recipients. By employing new techniques of T1 mapping, MRI scanning can assess the space between myocardial cells. This space, called the extracellular volume, is increased when there is inflammation. Inflammation may also be detected by myocardial T2 mapping with T2 values increased in regions of myocardial rejection. Dr. Samyn was enthused by the innovative properties of MRI, and the idea for this grant was born.
The trial will enroll 70 pediatric heart transplant patients with acute rejection and 130 healthy pediatric heart transplant patients without rejection. “Patients will be recruited from collaborating sites across the United States,” Dr. Samyn stated. “Right now, we have 16 cardiac centers supporting this research. Patients will still undergo the catheter-based heart biopsy which is the current standard of care but will also have a cardiac MRI, so the results of the two can be compared.”
At the time of catheterization, the study’s subjects will provide a blood sample to assess cell-free DNA (cfDNA) and micro RNA, novel biomarkers associated with rejection. The cfDNA work is performed in the Mitchell Lab at the Medical College of Wisconsin due to the pioneering research of Aoy Tomita-Mitchell, PhD, a professor at the Medical College of Wisconsin, and Michael Mitchell, MD, surgical director at the Herma Heart Institute. The decision to include the Mitchells’ research was an easy one, according to Dr. Samyn. “I thought, how can we make our project more interesting and dovetail on something that’s already been done at our institution in an area where we have a wealth of knowledge and expertise,” she said.
Finally, microRNAs in the blood, which are noncoding RNAs that play important roles in regulating gene expression, will also be evaluated for signs of rejection. The novelty of these other approaches, she suspects, made the grant more interesting to the NIH.
So, might biopsies for heart transplant patients eventually become a thing of the past and rejection only assessed with noninvasive options like MRI and a blood test? “I think it’s going to take time for the scientific world to accept that,” she said, “but I’m hopeful this research will be a step in that direction.”


Spotlight on Janette Strasburger, MD
Spotlight on Janette Strasburger, MD
Improving fetal health
It’s been a busy year for Janette Strasburger, MD, pediatric cardiologist at Children’s Wisconsin and researcher and professor of Pediatric Cardiology at the Medical College of Wisconsin. Her lab explores the use of fetal magnetocardiography (fMCG) to detect life-threatening fetal arrhythmias, allowing for early intervention.
This technology saves lives. Although the technology was FDA-approved in 2016, its use has been limited by the significant capital investment required for the shielded room that houses the machine as well as the cost of fMCG itself. Children’s Wisconsin is one of only a handful of centers with the technology. But that’s about to change.
Thanks to a $1.6 million National Institutes of Health (NIH) grant, Dr. Strasburger, together with the UW Madison Biomagnetism Laboratory and Applied Physics Systems, Inc, a Silicon Valley company that specializes in fetal heart rhythm recording, may have a smaller, less expensive fMCG ready for testing in early 2023. It is expected to cost far less than the current technology and provide higher resolution with a smaller footprint.
Dr. Strasburger and her team published several papers this year attesting to the ability of fMCG to identify silent arrhythmias that can be medically managed. In a paper to be published in the Journal of the American College of Cardiology: Clinical Electrophysiology,1 a retrospective review of 33 pregnant women whose fetuses had congenital heart defects or cardiomyopathy found that 45 percent had at least one significant new finding using fMCG that hadn’t been seen on echocardiography. Most could not have been identified on echo alone. The additional findings led to management changes in 30 percent of those patients.
In a second major paper, published in the Journal of the American Heart Association, Dr. Strasburger and her co-investigators reviewed fMCG tracings and medical records of 215 pregnancies referred to the Biomagnetism Laboratory because of fetal arrhythmia or risk of arrhythmia over the past 10 years.2 They assessed the referral diagnosis and treatment in 144 fetuses with tachycardia, bradycardia/AV block and familial long QT syndrome. The fMCG resulted in additional findings in 81 percent of patients, 56 percent of which were critical. These resulted in management changes in 76 percent of the cohort, 24 percent of which were major.
“These are huge impacts in medicine,” said Dr. Strasburger. “Similar results are emerging in the use of fetal MRI for heart and brain function. The implementation of MCG and MRI is having a huge impact on care.” That’s because many fetal arrhythmias and other congenital conditions can be addressed with prenatal therapies in the second or third trimester, reducing the risk of death.
In 2022, Dr. Strasburger spoke at a U.S. Food and Drug Administration (FDA) seminar on fetal pharmacology and to the NIH’s quantum subcommittee, which highlighted her work in using quantum sensors, a critical component in fMCG. In January, she co-chaired for the first NIH Public Seminar on Quantum Sensing Technologies. “Both the FDA and NIH are now recognizing the importance of this quantum science technology to improve fetal health,” she said.
1 Wacker-Gussmann A, Strasburger J (Co-First Author), Wakai RT.
Fetal Magnetocardiography Alters Diagnosis and Management in Fetal Congenital Heart Disease and Cardiomyopathy. J Am Coll Cardiol EP. 2022 Sep;8(9):1159-1161. https://doi.org/10.1016/j.jacep.2022.04.012.
2 Wacker-Gussmann A, Strasburger JF, Wakai RT. Contribution of Fetal Magnetocardiography to Diagnosis, Risk Assessment, and Treatment of Fetal Arrhythmia. J Am Heart Assoc. 2022;11(15):e025224.


Spotlight on Joy Lincoln, PhD
Spotlight on Joy Lincoln, PhD
An innovative use for cord blood
What if you could use a baby’s own stem cells from their umbilical cord to cure their congenital heart condition? That’s the Holy Grail for Joy Lincoln, PhD, who, with her team, is working closely with Aoy Tomita-Mitchell, PhD, a professor at the Medical College of Wisconsin, and Michael Mitchell, MD, surgical director at the Herma Heart Institute, to reach that goal.
Dr. Lincoln enrolled the first patient in the study in March. Since then, the number of participants has grown exponentially, thanks to her work in partnering with organizations like Conquering Congenital Heart Disease, which published her article on the topic.
Her team has already isolated mesenchymal stem cells, which can differentiate into a variety of organ cells, including cardiac cells, and endothelial progenitor cells, which are important in repairing the endothelial lining of blood vessels.
“We’re focusing on using the patient’s own umbilical-derived mesenchymal stem cells to promote the differentiation toward cardiac cell types,” said Dr. Lincoln. “One goal is to create a surgical material patch of a beating heart muscle that can then be transplanted back into the patient.”
One use could be for babies born with hypoplastic left heart syndrome, who must undergo three surgeries in just the first five years of life. “The goal would be to use these patient’s own cells to minimize the number of surgeries they need,” said Dr. Lincoln, thus reducing the risks of surgery and associated complications.
At the same time, the team is using those cells to better understand the genetic cause behind the disease. “Why did that genetic defect cause disease?” Dr. Lincoln asked.
In fact, the team identified a genetic mutation in one newborn that prevented the cardiac cells from beating normally. They are now using the baby’s cells as a platform to test different drugs to see if they can overcome the genetic mutation. “We know there are drugs on the market that improve contractility of the heart,” said Dr. Lincoln. If they find one that is effective, it could help resolve the baby’s rhythm problem.
With the endothelial progenitor cells, the lab is working closely with the team to create a tissue-engineered heart valve. “Right now, we’ve progressed to the level where we’re comparing how much endothelial progenitor cells mimic those from human heart valves,” she said. In other words, how close are they to a real human heart valve cell? Do they express the same genes?
“Once we have that, we’ll seed these cells onto different scaffolds to make the tissue-engineered heart valve,” she said.

Studying heart cells

Lu Han, PhD
Lu Han, PhD
Lu Han, PhD, receives Michael H. Keelan, Jr., MD Scholar award
Lu Han, PhD, researcher at the Herma Heart Institute and assistant professor of Pediatric Cardiology at the Medical College of Wisconsin, received the 2022 Michael H. Keelan, Jr., MD Scholar award from the Medical College of Wisconsin.
Her project, titled “Exploring the mechanisms promoting human iPSC-derived cardiomyocyte maturation,” aims to better understand the mechanisms that regulate the dynamics of heart muscle (cardiomyocytes) in physiological and pathological growth of the heart, in order to advance the development of new treatments for congenital and adult disease.
Her research is principally interested in cell proliferation and differentiation in the context of heart development. “We want to understand how the heart muscle cells differentiate and proliferate, therefore affecting heart regeneration,” she said. “This is the big scheme of our research.”
Dr. Han’s project will endeavor to produce induced pluripotent stem cells (iPSC)-derived cardiomyocytes that closely resemble naturally existing cells within the adult human body in terms of structure and function. As these synthesized heart muscle cells can still show some differences with cells directly obtained from humans, she hopes “to understand whether there are some particular parameters that can contribute to the cell maturation.” The objective is to produce optimized cells that will allow scientists to test ideas and develop novel treatments for humans.
This research holds enormous promise for the future of personalized medicine, drug testing and regeneration therapy.

New faculty
Children's welcomes the following faculty members to the Herma Heart Institute
Problem-solving mindset

Tracy Geoffrion, MD, MPH
Tracy Geoffrion, MD, MPH
Welcome Tracy Geoffrion, MD, MPH
Ever since she was a little girl growing up in East Texas, Tracy Geoffrion, MD, MPH, knew that she wanted to be a doctor. “I can remember being a kid and thinking that my pediatrician had a really cool job,” she said.
Now, after years of studying and gaining professional experience, Dr. Geoffrion has joined the Herma Heart Institute at Children’s Wisconsin as a pediatric cardiothoracic surgeon and an assistant professor of Congenital Heart Surgery at the Medical College of Wisconsin.
EDUCATION AND TRAINING
Dr. Geoffrion received her bachelor’s degree in economics from Vanderbilt University before pursuing a master’s degree in Public Health from Dartmouth Medical School. She then returned to her home state to complete her medical degree at the University of Texas in San Antonio.
Until that point, she thought she wanted to study obstetrics and gynecology. But in medical school, she discovered that she loved the task-oriented, technical aspects of surgery. She also enjoyed being able to identify a problem and solve it by performing a specific procedure. “I felt like I had made a very concrete difference in a patient’s life, and there was something really special about the bond between a patient and a surgeon,” she said.
Dr. Geoffrion went on to study surgery and adult cardiac surgery at the UT Southwestern Medical Center in Dallas. She joins Children’s Wisconsin from Children’s Hospital of Philadelphia, where she completed a year of accredited congenital cardiac surgery, another year as a general cardiac surgeon and, finally, a year serving as a surgery instructor and doing a postdoctoral research fellowship.
ADVENTUROUS SPIRIT
Dr. Geoffrion had never visited Wisconsin before interviewing with Children’s, and she’s looking forward to exploring her new home.
“I like an adventure, and I consider this to be an adventure,” she said of the move. In her free time, she enjoys traveling, weightlifting, hiking and skiing. And she loves a good adrenaline rush. Before attending medical school, she even considered going into the military to fly fighter jets because of the excitement and technical skills required. But not all her interests are about seeking thrills — she’s also a classically trained singer.
The Children’s Wisconsin community has welcomed Dr. Geoffrion with open arms. “I’m excited to be here, to get to know the Midwest and to take care of the patients in this community,” she said.
Graduated fellows
Children's congratulates our graduated fellows
Adedotun Adewale, MD, MPH, completed his pediatric cardiac critical care fellowship at Children’s Wisconsin. He is now on faculty at St. Louis Children’s Hospital.
Hugh Bigg, DO, completed his pediatric cardiology fellowship at Children’s Wisconsin and is in an advanced imaging fellowship at Arkansas Children’s Hospital.
- Academic product: “Prognostic Utility of Echocardiographically Derived Left Ventricular Strain in Assessing Neonatal Enteroviral Myocarditis Outcome”
Chalani Ellepola, MD, completed her advanced imaging fellowship at Children’s Wisconsin. She is currently a pediatric cardiologist and imager at Texas Children’s Hospital in Houston.
- Academic product: “Limitations of Predicting Postoperative Left Atrioventricular Valve Regurgitation by Intraoperative Transesophageal Echocardiography”
James Kimber, DO, completed his fellowship in Adult Congenital Heart Disease at Children’s Wisconsin. He is now on faculty at Penn State in Hershey, PA.
Sheena Mansukhani, DO, completed her pediatric cardiology fellowship at Children’s Wisconsin and will be starting an advanced imaging fellowship in 2023 in Chicago.
- Academic product: “Factors Associated with Interstage Feeding Outcomes in Infants with Hypoplastic Left Heart Syndrome Undergoing Norwood Palliation”
David Segar, MD, completed his pediatric cardiology fellowship and continues with an advanced imaging fellowship at Children’s Wisconsin.
- Academic Product: “The Relationship between Placental Pathology and Neurodevelopmental Outcomes in Complex Congenital Heart Disease”
We welcome the opportunity to partner with you to serve your patients and deliver the very best outcomes possible.
We are happy to answer any questions through our physician referral access center by phone or by email: (414) 266-6457 or heart@childrenswi.org. We are also available to discuss second opinion cases at heartconnect@childrenswi.org.





