Shaping the future of pediatric heart care
Understanding the root causes of congenital heart disease (CHD) in each of our patients and creating personalized lifelong treatment plans requires a collaborative multidisciplinary approach — this is the cornerstone of our cardiac program.
Teamwork and collaboration have always been and continue to be an important part of the work we do each and every day to support the patients and families of the Herma Heart Institute and provide the best and most comprehensive, coordinated and patient-centered care. This year has been no exception. In fact, our 2024 accomplishments demonstrate the power of collaboration and its impact on innovation and advancements in research and patient care.
Our program continues to support cutting-edge science and quality improvement and outcomes studies that advance the care we provide our patients and families in various stages of the life cycle — from fetal into adulthood. In 2024, we supported many multidisciplinary studies, including the expansion of the Educational Achievement and Partnership Program in its efforts to advance lifelong learning and educational attainment for kids with chronic illnesses. We also continue to support the careers of promising junior physicians with research interests and create opportunities to address new initiatives. In 2024, this included programs assessing the physical activity needs of kids with complex CHD, advancing surgical innovations using patient-specific imaging to generate 3D individualized anatomical models for improved planning and outcomes and enhancements to our Norwood pathways. The Herma Heart Institute takes enormous pride in participating in new and compelling initiatives that have the potential to improve the lives of the children of Wisconsin and beyond. The combination of committed institutional investment along with the “team science” culture has significantly leveraged our success in securing extramural funding, making us one of the leading heart institutes for quality, outcomes and research in the nation.
As the Herma Heart Institute steps into the next era of growth, we are deepening our commitment to our mission of advancing patient care while strengthening our infrastructure. We are fortifying our roots to support the program’s planned advancements and increasing collaborations to improve the physical, social and mental health of kids born with structural cardiovascular anomalies. Over the next few years, we plan remarkable new initiatives to further leverage our cardiovascular precision medicine program that includes expansion of our patient biobank and tissue engineering developments.
Together, we are grateful for the opportunity to lead a program that trains the next generation and serves cardiac patients and families in Wisconsin.
Joy Lincoln, PhD
Director of cardiovascular research
Herma Heart Institute

Fueling progress: The Herma Heart Institute’s commitment to innovation and research
The Herma Heart Institute (HHI) Innovation Fund was established in 2018 with the goal of advancing research, driving quality improvement initiatives and promoting innovation in cardiovascular education and training. This year, eight grants were awarded for research and quality improvement studies.

2024 Innovation Fund Award winners
Joy Lincoln, PhD, drives innovation and discovery though her cardiac precision medicine work, studying the function and mechanics of bicuspid aortic valves in her lab at the Children's Research Institute.
Joy Lincoln, PhD, drives innovation and discovery though her cardiac precision medicine work, studying the function and mechanics of bicuspid aortic valves in her lab at the Children's Research Institute.
HHI Innovation Fund research and quality improvement grants
Project RECESS: Reimagining EAPP’s continuum of service for equity, effectiveness, efficiency, satisfaction and sustainability — Christie Ruehl, JD, MBA, and Kyle Landry, MEd
In Reimagining the EAPP’s continuum of service for equity, effectiveness, efficiency, satisfaction and sustainability, Project RECESS will align the Educational Achievement Partnership Program (EAPP)'s purpose, function and services under a new dynamic empowerment system where the EAPP shifts from the role of information hub to care coordination coach. The overall goal of Project RECESS is to improve program outcomes, efficiency and sustainability by coaching families to become the project manager of their children’s future medical-school-home-community care coordination. Project results will yield preliminary data needed to establish a sustainability plan, pursue long-term program funding, guide further program development and redefine staffing needs as services expand systemwide.
Vascular inflammation in single ventricle pulmonary arteriovenous malformations — Andrew Spearman, MD
The objective of this pilot proposal is to determine whether increased lung macrophages are a primary or secondary component of pulmonary arteriovenous malformations (PAVM) pathophysiology. Accomplishing the objective of this proposal will lead to new scientific knowledge and potentially identify new therapeutic targets in single ventricle PAVMs. With the help of this pilot study, the team has already leveraged their findings for extramural funding to longitudinally and mechanistically study vascular inflammation and therapeutic immune modulators in PAVM pathogenesis.
Monocytic ACE2 and extracellular matrix remodeling in Kawasaki disease — Rodney Willoughby, MD
Kawasaki disease, the most common acquired heart disease of children in World Health Organization (WHO) Tier 1 countries, remains unexplained after 50 years. The team found that monocyte expression of ACE2, MMP-9 metalloprotease, TIMP-1 cytokine and PIIINP peptide are all altered during COVID-19 morbidity. We will test by case-control design whether these cellular components of the renin-angiotensin system (RAS) and evidence of vasculitis, cytokine-driven inflammation and fibrosis at onset of COVID-19 might also promote the pathogenesis of the pediatric post-COVID-19 syndrome (MIS-C) and, by extension, Kawasaki disease. This study will justify much larger epidemiological and laboratory grants to confirm these systems in the causal pathway to Kawasaki disease.
Herma Heart Institute seed grants
MIKE’s HEART (Making an impact in kid’s exercise: health education, activity, and rehabilitation team) — Michael Danduran, MS, PhD
This project will address the physical activity needs of young children with congenital heart disease, identify deficits in physical development, prevent the noted declines in exercise capacity, and address the patient’s/parent’s fears and apprehensions regarding safe participation.
Exploring patterns of psychological traits and health-related quality of life in teenagers with congenital heart disease — Tracy Geoffrion, MD, and Vanessa Aguilera Snyder, PsyD
There is substantial research highlighting the neurodevelopmental and psychological sequelae of cardiac surgery in infancy. These sequelae have been found to impact health-related quality of life (HRQOL) for school-aged youth. While there is some research assessing possible predictive factors of HRQOL in youth with CHD, there is limited research assessing specific psychological traits as predictors of HRQOL, particularly in teenage patients. Results from this project will allow for more targeted support and interventions to improve HRQOL in this patient population.
When do hepatic biomarkers and cytokines peak post-high-intensity exercise in patients with Fontan circulation? — Alexis Gumm, MD
After conducting a pilot study at Children’s Wisconsin with 10 patients post-Fontan surgery, we assessed for acute liver injury following high-intensity exercise. The study revealed a small but statistically significant increase in ALT levels as well as pro-inflammatory cytokines post-exercise. However, these blood samples were taken within 40 minutes of completing the exercise. Given that the half-life of ALT is 47 hours, and studies assessing ischemic-reperfusion liver injury find AST/ALT >1000 IU/L within three hours of injury, I hypothesize that our labs were drawn too soon to see the peak rise post-exercise. Before pursuing a large prospective exercise study, this study aims to scientifically find the peak of these biomarkers and cytokines, post-exercise, with a small pilot study of 10 patients to determine when we should be drawing blood post-exercise in these patients.
Therapeutic testing in a rat model of Glenn circulation — Andrew Spearman, MD
This pilot project will directly test whether anti-inflammatory therapies can modify initiation and progression of pulmonary arteriovenous malformations (PAVMs) after Glenn surgery. We are using clinically available and research-only drugs to study how inhaled and systemic drugs can modify single ventricle PAVMs. Findings from this pilot project will advance our knowledge of single ventricle PAVMs and the field of vascular biology in general.
Optimizing resiliency in congenital heart disease (ORCHD) — Kathy Miller, MBA, RN, BSN, Michelle Loman, PhD, Sara Markuson, PhD, and David Segar, MD
In addition to the neurodevelopmental and mental health concerns for children with CHD, research suggests that the medical complexity associated with CHD can result in elevated illness-related parenting stress for caregivers. Clinically, we have observed a pattern whereby caregivers of children with CHD seem to have different, typically lower, expectations for and perceptions of their child’s daily living skills than age-matched peers without CHD. In order to optimize resiliency in children with CHD and their families, our research project aims to develop and validate a parent report measure which adequately assesses parental expectations for and perceptions of child functioning. It will also assess the relationship between child and family factors and parental expectations and perceptions of their child’s functioning.
HHI and Advancing a Healthier Wisconsin pilot grant
Evaluating the efficacy of human recombinant dornase alfa on cell-free DNA concentration — Justinn Tanem, MD
Circulating cfDNA is released into the blood due to normal cell turnover and apoptosis, and monitoring concentrations has shown promise for clinical utility in a variety of disease states. Animal models have shown DNase 1 to be an effective scavenger of cfDNA, with improved outcomes. Our hypothesis is that Pulmozyme will result in a significant decrease in the concentration of cfDNA.
We also want to take a moment to give recognition to all of our dedicated staff and researchers whose outstanding work has garnered significant funding to help them pursue innovation and discover breakthroughs.
Kasey Chaszczewski, MD
REVISIT-3D (Real-time segmentation, virtual image modification, surgical intervention modeling and 3D printing for improved preoperative surgical preparedness and acute outcomes) — Project Bubaloo
Tracy Geoffrion, MD
Cardiac sarcomere gene variants in congenital heart disease — American Academy of Thoracic Surgeons Foundation
John LaDisa, PhD
Mechanical stimuli as a predictor of adverse outcomes after pulmonary vein stenting — NIH National Heart, Lung and Blood Institute
Joy Lincoln, PhD
Characterization of an isoform-specific anticoagulant function of TFPI-alpha — NIH National Heart, Lung and Blood Institute
Joy Lincoln, PhD, and John LaDisa, PhD
Bicuspid aortic valve biomechanics and calcification — NIH National Heart, Lung and Blood Institute
Christie Reuhl, JD, MBA, and Kyle Landry, MEd
Project iSERVE: Investigating service effectiveness, reliability and validity for equity — Advancing a Healthier Wisconsin
Andrew Spearman, MD
Longitudinal analysis of single ventricle PAVM pathophysiology — Additional Ventures
Janette Strasburger, MD
Safer medication treatment during pregnancy using Fetal MCG and pharmacological modeling — Advancing a Healthier Wisconsin
Enhancing preoperative planning with 3D visualization
For decades, cardiothoracic surgeons have relied on echocardiography, CT scans and MRIs to plan their surgical approach. Now virtual reality and 3D modeling are transforming the Herma Heart Institute’s preoperative planning process.
Virtual reality is nothing new for the Herma Heart Institute — in 2018, it became one of the first sites to pioneer the use of the Stanford Virtual Heart as a virtual reality education tool for providers and patients to explore different heart defects in an immersive environment. We also used virtual reality to provide an immersive experience during the Heart Summit, where a group of some of the world’s greatest medical minds gathered to watch an open-heart surgery live in 3D while interacting in real time with the surgeon.
Kasey Chaszczewski, MD, and Ben Goot, MD, use virtual reality and 3D modeling to analyze a patient's heart.
Kasey Chaszczewski, MD, and Ben Goot, MD, use virtual reality and 3D modeling to analyze a patient's heart.
Then in 2023, cardiothoracic surgeon Michael Mitchell, MD, asked the team’s 3D experts — biomedical engineer John LaDisa, PhD, and pediatric cardiologists Kasey Chaszczewski, MD, and Ben Goot, MD — to model some complex surgical baffle repairs. The trio used the patients’ cross-sectional imaging to create a virtual reality model and then a printed model, which they presented at the next week’s surgical conference. The cardiology and surgical teams were so excited about the possibilities that the Herma Heart Institute decided to embrace 3D modeling as a part of standard preoperative preparation for complex surgical cases.
“The 3D reconstructions have been very helpful in developing a targeted approach to the operation,” said Dr. Mitchell, division chief of pediatric cardiothoracic surgery at Children’s Wisconsin and co-surgical director of the Herma Heart Institute. “We determine what is possible and what is most optimal, and then it makes the operation itself a lot more facile because we have a really good understanding of what we can accomplish anatomically and what pitfalls to watch out for.”
In the past year, the Herma Heart Institute has modeled 10 cases in virtual reality, and with funding from Project Bubaloo, the team recently invested in new 3D software.
“Our goal is to inform surgical decision-making so that we minimize the surprises for the surgeon and help them lay out the best game plan before going into the operating room,” said Dr. Chaszczewski. “We will model where a patch might go in a surgical procedure and can see what the heart would look like after a proposed surgical intervention. In certain cases, we’ve identified that a particular surgery is not the best option and that we need to pursue a different strategy.”
It’s a huge step up from the 2D images that surgeons have traditionally used to inform their planning. “Creating a 3D model eliminates variability when it comes to creating spatial recognition in your head and allows everyone to be able to visualize where a patch might be placed, where an additional connection might be, and where problems in the operating room might arise.” said Dr. Chaszczewski.
The 3D modeling is particularly helpful for determining the best surgical approach for double outlet right ventricle cases, which can be repaired in different ways depending on the patient’s anatomy.
The team has also used the technology to plan complex intracardiac reconstructions that involve the pulmonary veins, Ebstein malformation of the tricuspid valve, repair of the mitral valve in patients with Shone’s complex or small left-sided structure and complete atrioventricular canal defects.
“Our goal is to continue to identify specific anatomic pathologies that might benefit from this technology,” said Dr. Chaszczewski.
While more pediatric centers are beginning to embrace virtual reality for preoperative planning, there’s more to be done on the research side to demonstrate the clinical impact. One of the most important questions that the Herma Heart Institute team is trying to answer: how do you quantify whether 3D modeling is making a difference?
“This is actually a hard question to answer,” said Dr. LaDisa. “But we’re putting a fair
amount of time into specking out quality improvement and research-based activities that will allow us to answer that question. We think that’s a way we can contribute to the field.”
The team also wants to identify which aspects of the models are most helpful to surgeons and then refine those features so that they’re even more effective.
In the meantime, the Herma Heart Institute’s surgeons are grateful for the enhanced perspective.
“It gives you a big advantage because you can see in advance some of the details and some of the relationships with a higher degree of accuracy. It allows us to do the next generation of repair work with a very careful, well-thought-out plan,” said Dr. Mitchell. “And with the advantage of having time to prepare in advance, I think we get much better results than if we’re making all of the decisions for the first time on the operating table.”
Questions about our 3D visualization work? Please email us at hermaheartinstitute@childrenswi.org.

Detecting fetal arrhythmias
Developments in technology and holistic care for high-risk pregnancies
Many of the 21,000 stillbirths each year in the United States are likely due to unrecognized fetal heart conditions, according to Janette Strasburger, MD, a pediatric cardiologist at the Herma Heart Institute. In partnership with the University of Wisconsin School of Medicine and Public Health, Dr. Strasburger helped to pioneer fetal magnetocardiography (fMCG). This groundbreaking technology, performed at the University's imaging facilities, detects life-threatening heart rhythm disorders in unborn babies and enables early intervention. “Our long-term goal is the prevention of, or at least the reduction of stillbirth,” she said.
Helping moms and their babies
The Fetal Heart Program at the Herma Heart Institute sees about 700 patients (pregnant women and their babies in utero) a year and partners closely with the Children’s Wisconsin Fetal Concerns Center. “Usually, there is some kind of congenital heart concern, and many are being referred due to specific diagnoses,” said Sara Creighton, MD, a pediatric and fetal cardiologist.
The Fetal Heart Program uses a standardized tool to indicate the level of care that will be needed once a child is born, whether the delivery takes place at the Froedtert Hospital Birth Center, which is next door to Children’s Wisconsin, or elsewhere. The level can range from a typical newborn nursery to a neonatal intensive care unit to dual operating rooms for a baby to have surgery immediately following a C-section. Such standardization helps remove the burden from medical centers so they know how to respond right away, and it also helps improve the system for moms so they know what to expect after delivery. “We are a model for other programs about how to approach care at a distance for patients who may not live near the main campus,” Dr. Creighton said.
The program is also a model for how to treat patients.
“The multidisciplinary collaboration with our Fetal Concerns Center and our ability to provide regional care for our patients are two things that set our program apart,” said Dr. Creighton. Once fetal heart issues are identified using ultrasound, sometimes augmented by fMCG technology, “we can provide comprehensive services for patients that can help predict the safest care for them. It can bring the mom, baby and medical component all together with a holistic experience that takes care of them as a family.”
How Children’s Wisconsin uses fMCG
With the use of fMCG, “we have found that with patients who come to be evaluated, there is at least a 50 percent chance we will find something in addition to or that will alter a diagnosis that has been made by ultrasound, and that leads to changes in management in almost 25 percent of patients,” said Dr. Strasburger.
Knowing more about a baby’s heart issues while in utero helps parents better prepare for life after birth. The Fetal Heart Program, which includes Dr. Strasburger, Dr. Creighton and three other fetal cardiologists, as well as ultrasound and nursing staff, works with obstetricians to discuss fetal concerns. When appropriate, they refer patients to social workers, lactation consultants, child life specialists and other ancillary services for pregnant and postpartum women. This helps patients find the care they need, either at Children’s Wisconsin or their home hospitals if they have traveled for their fetal heart care. Patients have come from as far away as Hawaii, Florida and Alberta, Canada.
Innovation beyond Children’s Wisconsin
Looking ahead, Dr. Strasburger wants to see more mothers and their babies benefiting from fMCG technology. To do so, she, her collaborator in medical physics, Ronald T. Wakai, PhD, from the Biomagnetism Laboratory at the University of Wisconsin School of Medicine and Public Health, and her team are involved in research to make it accessible to more pediatric cardiologists and maternal-fetal medicine specialists. Currently, the Fetal Heart Program uses a Superconducting Quantum Interference Device (SQUID) to detect fetal heart arrhythmias using fMCG technology. The FDA-approved device is cooled with liquid helium, which is both costly and rare. As a result, this fetal heart monitoring can’t be universally implemented.
Dr. Strasburger’s lab is collaborating with a California tech company to develop a similar, more affordable device called optically pumped magnetometry (OPM) with a $1.66 million NIH small business innovation research grant. The OPM device would replace the SQUID device, making fMCG technology easier to offer in more locations around the world. Doing so would help identify fetal cardiac issues in more babies in utero and would, in turn, likely lead to a reduction in the current stillbirth rates, as Dr. Strasburger cites in interviews.
Having more fMCG available would also help mothers get the care they need closer to their homes, said Dr. Strasburger. “Over two-thirds of our patients are coming to us from further than 100 miles away to get this test,” she said. “It’s important that we get this technology in other hospitals so we can get these moms off the road and into the safest place for them to be.”

New interest fuels Project ADAM’s growth
When NFL player Damar Hamlin suffered a sudden cardiac arrest in the middle of a game in 2023, millions watched on TV as medical staff sprang into action and successfully saved his life with CPR and an automated external defibrillator (AED). The dramatic scene illustrated what Project ADAM leaders at the Herma Heart Institute and affiliates across the country already knew: planningand training for cardiac emergencies is critical in protecting children and adults from sudden death.
“Our work has always been important and has been recognized for years,” said Alli Thompson, the national and Wisconsin administrator for Project ADAM, which works to equip and prepare schools for sudden cardiac emergencies. “But the Damar Hamlin event took it to another level and truly shined a spotlight on the importance of Project ADAM’s work.”
Project ADAM (Automated Defibrillators in Adam’s Memory) started in 2000 after 17-year-old Wisconsin native Adam Lemel died from sudden cardiac arrest during a high school basketball game. At that time, AEDs were not accessible in schools, and prompt bystander CPR was often delayed because sudden cardiac arrest was not always recognized as the cause of sudden collapse and apparent seizures.
The organization’s growth has accelerated in recent years, and now there are 45 affiliate programs across 33 states. In 2024, Project ADAM partnered with more than 1,800 new schools and trained more than 7,000 school staff in how to respond to cardiac emergencies.
But perhaps the most meaningful metric is how many lives have been saved since Project ADAM began at the Herma Heart Institute in 2000 — more than 250 and counting.
“At least half of the people whose lives have been saved are adults, so this program is not just for kids,” said Anoop K. Singh, MD, Project ADAM’s medical director and medical director of pediatric cardiology at Children’s Wisconsin. “Schools are really a hub for all people. It’s estimated that on any given day, 20 percent of the U.S. population is in a school.”
Survival rates for sudden cardiac arrest are typically around 10 percent, but in schools that are prepared, the survival rate approaches 70 percent. This past year, a Milwaukee Public Schools teacher at 95th Street School, a Project ADAM Heart Safe School, was saved by quick-thinking colleagues when she collapsed suddenly in her classroom after coming in from a fire drill. In the 11 minutes it took for emergency medical services to arrive on the scene, the teacher’s colleagues administered CPR and delivered a shock from the school’s AED, saving her life.
AED legislation has also become a hot topic since Damar Hamlin’s collapse on national TV. Project ADAM has joined the National Football League, American Heart Association and other organizations in the Smart Hearts Sports Coalition. The coalition is advocating for all 50 states to adopt legislation to implement evidence-based policies that could prevent sudden cardiac death in high school students. Already this year, Michigan and Tennessee have enacted related legislation, and efforts are underway in other states, including Wisconsin.
“This national movement presents a great opportunity in Wisconsin to advocate for the protection of our students, staff and visitors in the event of a sudden cardiac arrest, as there is currently limited legislation related to access to AEDs for schools and athletics,” said Thompson. “I think we’re going to start to see some impactful legislation that strengthens the work that Project ADAM has been committed to for decades.”

Improving care for coarctation of the aorta
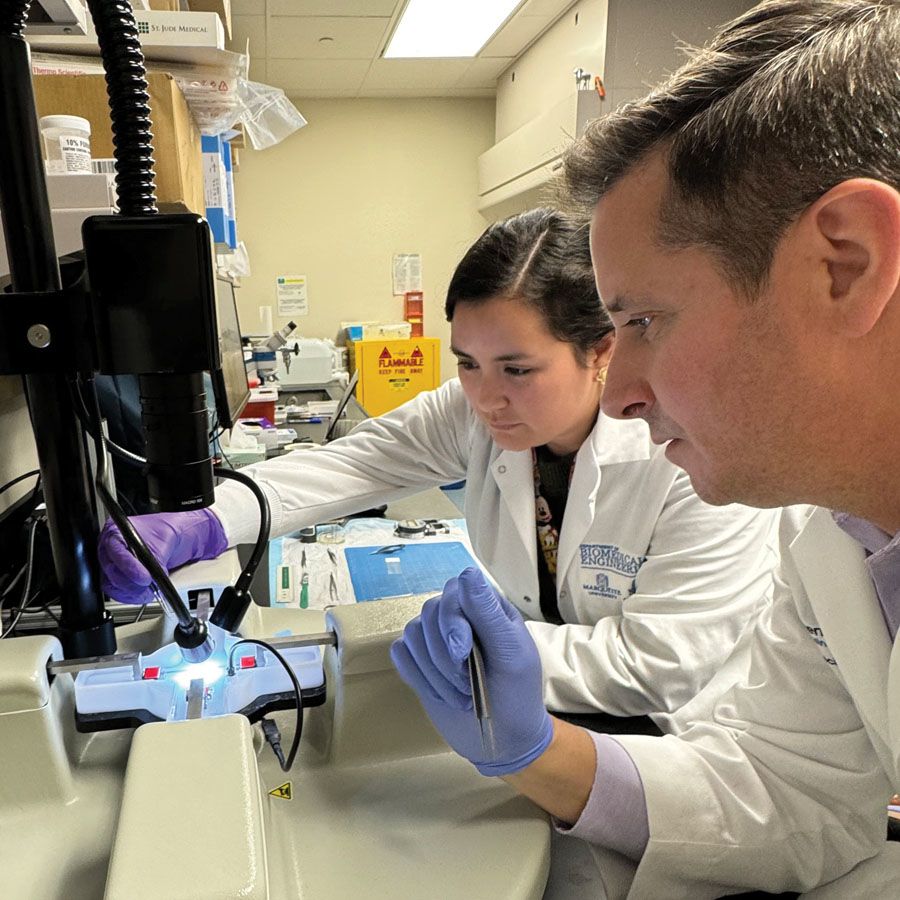
John LaDisa, PhD, evaluates data from his latest research, studying changes in stiffness from coarctation of the aorta that may lead to hypertension.
John LaDisa, PhD, evaluates data from his latest research, studying changes in stiffness from coarctation of the aorta that may lead to hypertension.
Up to 80 percent of children with coarctation of the aorta (CoA) will develop hypertension 25 years after surgical repair. After years of trying to unravel the reasons why, Herma Heart Institute researcher John LaDisa, PhD, has discovered new clues about which children are more likely to develop problems.
Dr. LaDisa, a biomedical engineer, has studied the mechanics of CoA for two decades. With support from a $1.5 million grant from the National Institutes of Health (NIH), he published his findings from a preclinical model in Hypertension earlier this year.
“We wanted to try to understand why so many of these children are still hypertensive despite early correction in many cases and later correction in others,” said Dr. LaDisa. “And we’re taking aim at the current guideline, which doesn’t have great evidence to back it.”
The current guideline calls for intervening when a child’s blood pressure gradient is above 20 mmHg. “These kids are still becoming hypertensive,” said Dr. LaDisa, “so that underscores to me that it’s probably not the right number, and it’s probably multifactorial.” The LaDisa Lab has been systematically studying how long the blood pressure gradient has been at that level, and when it presented itself, in hopes of improving the guideline.
One surprise from Dr. LaDisa’s preclinical model was that the aorta didn’t revert back to baseline, even when it was only temporarily narrowed — it still showed signs of thickening, stiffening and dysfunction. Through his research, he has concluded that intervening earlier, at a less severe disease stage, would prevent the aorta from permanently remodeling itself.
“We want to try to figure out when things are no longer reversible and make sure that we’re ultimately treating kids before that happens,” he said.
Dr. LaDisa also previously collaborated with the lab of Aoy Tomita-Mitchell, PhD, and Michael E. Mitchell, MD, to study gene expression changes involved in CoA, ultimately leading his team to look more closely at natriuretic peptide receptor-C, or NPR-C.
“It turns out that this gene and the associated protein are having an impact on the physiology of the aorta. That was another piece of the puzzle,” said Dr. LaDisa, who plans to continue to explore the role
of NPR-C.
He recently received a $2.3 million grant from the NIH to advance the next stage of his CoA research. For that project, he is building on his findings from the preclinical model by analyzing retrospective data from over 1,000 CoA patients across four clinical sites: Children’s Wisconsin, American Family Children’s Hospital in Madison, Wis., C.S. Mott Children’s Hospital in Ann Arbor, Mich., and UF Health Shands Children’s Hospital in Gainesville, Fla.
John LaDisa, PhD, and Carla Guzman, MD, postdoctoral scholar at the Medical College of Wisconsin, study tissue samples in the lab.
John LaDisa, PhD, and Carla Guzman, MD, postdoctoral scholar at the Medical College of Wisconsin, study tissue samples in the lab.
The goal is to look at when children had a surgical repair and at what coarctation severity to determine which patients were more or less likely to develop hypertension later in life. That data could inform new, more effective intervention guidelines.
“We’ll be fine-tuning what we hope will ultimately lead to improved treatment guidance,” he said. “We really want to help kids, and we think this is an area where we can make an impact.”
For more information about this research work, please email hermaheartinstitute@childrenswi.org.
Grateful family spotlight
A heartfelt mission
Project Bubaloo was founded by local mother Callie Chiroff in honor of her son Theo James “Bubaloo” Schlicht, who was a patient at the Herma Heart Institute. Since his passing, Project Bubaloo has raised more than $750,000 in support of research, education and awareness for congenital heart disease. Over the past year, a portion of these funds has been dedicated to enhancing both patient and staff education at the Herma Heart Institute.
Callie Chiroff, president and founder, and Katherine Jansen, vice president and CFO of Project Bubaloo, deliver developmental kits to the CICU at the Herma Heart Institute.
Callie Chiroff, president and founder, and Katherine Jansen, vice president and CFO of Project Bubaloo, deliver developmental kits to the CICU at the Herma Heart Institute.
Project Bubaloo was able to help fund Elemeno, a new tool for our cardiac intensive care unit (CICU) team that has made bedside education available for our staff and includes our Norwood pathway guidance, chest tube management, etc. They also helped fund a quality improvement project that equipped every room in the CICU with research-backed developmental kits.
A few Herma Heart Institute staff have received grants from the Project Bubaloo Research Fund. This past year, three different research projects were funded:
- Prevalence of MYH6 variants in congenital heart disease patients with heart failure — Tracy Geoffrion, MD, MPH, and Aoy Tomita-Mitchell, PhD
- Sedation practices in the CICU — Matthew Amidon, DO
- REVISIT-3D (Real-time segmentation, virtual image modification, surgical intervention modeling and 3D printing or improved preoperative surgical preparedness and acute outcomes) — Kasey Chaszczewski, MD, Benjamin Goot, MD, FASE, Michael Mitchell, MD, and John LaDisa, PhD
We are grateful to Project Bubaloo for all that they do to support our clinical and research teams in their drive to push innovation forward and provide the best and safest care for our patients.

Transitioning to new digital monitoring for interstage patients
More than 20 years ago, the Herma Heart Institute was the first pediatric cardiac program to develop and implement an Interstage Home Monitoring Program, aimed at increasing survival for babies with hypoplastic left heart syndrome (HLHS) and other single ventricle heart conditions. The Interstage Home Monitoring Program allows providers, with the help of parents/guardians, to track a patient’s oxygen saturation levels, feedings and weight and enables them to quickly identify any health changes that may require swift intervention.
“The Interstage Home Monitoring Program has allowed so many of our high-risk patients to develop, thrive and bond with their families in their home environment while also being closely monitored, which has reduced the risk of life-threatening complications,” said Stephanie Handler, MD, pediatric cardiologist and program director of the Interstage Home Monitoring Program at the Herma Heart Institute. The Interstage Home Monitoring Program has also been shown to improve nutrition and growth, neurodevelopment and overall survival, and is now a standard of care at cardiac centers both nationally and internationally.
Ryder Kintigh, one of our patients that went through the Interstage Home Monitoring Program, enjoys time with his family.
Ryder Kintigh, one of our patients that went through the Interstage Home Monitoring Program, enjoys time with his family.
Recently, the Herma Heart Institute implemented a new digital home monitoring platform. This secure, mobile, telehealth application allows for easy data entry, has Bluetooth capability for downloading weights obtained on the home infant scale, performs calculations related to feeding volumes and weight trends, and helps reduce the risk for errors. The platform also allows for HIPAA-compliant transmission of patient images and videos to the Herma Heart Institute Interstage team through an electronic medical record (EMR)-integrated application.
“This platform has been incredible," said Jena Tanem, APNP at the Herma Heart Institute. "Having all of this information at our fingertips has transformed the way we care for our single ventricle patients. Our provider teams are now able to view data in real time and promptly investigate any concerning clinical findings.”
This past year, the Herma Heart Institute Interstage Home Monitoring team presented 20 years of outcomes data related to their Norwood patients who were discharged into the program. Since 2005, they have not had any mortalities in their home-monitored patients. “As a clinician, it has been incredibly rewarding to witness not only the inception but also the transformation of the Interstage Home Monitoring Program over the last 24 years and see the positive impact that it has had on patients and their families,” said Nancy Rudd, APNP at the Herma Heart Institute.

Empowering patient families
at home and in the classroom
The Herma Heart Institute at Children’s Wisconsin launched the Educational Achievement Partnership Program (EAPP) in 2015 to advance long-term educational achievement in children with chronic illnesses and provide every child the opportunity to reach their optimal potential. While the EAPP started as a cardiology service, it began expanding to several additional pediatric populations in 2021. This past year, the program underwent significant restructuring to extend services hospital-wide and support children with all types of chronic illnesses. “The new vision for the program will allow us to support families across the state and nation by empowering parents and school staff with the EAPP’s best practice strategies for home, health and school care coordination,” said Kyle Landry, MEd, program manager of the EAPP.
Kyle Landry, MEd, and Christie Reuhl, JD, MBA, attend Pediatric Academic Societies (PAS) Annual Meeting to share information about the EAPP at Children's Wisconsin and collaborate with other health systems.
Kyle Landry, MEd, and Christie Reuhl, JD, MBA, attend Pediatric Academic Societies (PAS) Annual Meeting to share information about the EAPP at Children's Wisconsin and collaborate with other health systems.
As part of the program’s realignment, Children’s Wisconsin has joined seven other pediatric institutions as part of the nationwide School-Friendly Health Systems (SFHS) Collaborative, which strives to help children achieve optimal health and reach their full academic potential. Two of the values that are central to the SFHS framework, health care equity and shared power with families, were central pillars of the EAPP’s restructuring, which was funded with a Herma Heart Institute Innovation Fund grant and Advancing a Healthier Wisconsin grant. This funding supported two projects that have played a key role in driving the program’s evolution forward.
School-Friendly After Visit Summary Project
The EAPP has been working closely with cardiac physicians and nursing staff to develop a school-friendly after visit summary (SF-AVS) by adding a “what school needs to know” section — a streamlined way to give patient families information that will help school teams understand the child’s medical condition and health and learning risk factors. The SF-AVS also includes a “health-body-brain connection logic chain,” which explains the complex relationship between pediatric heart disease and physiological and neurodevelopmental sequelae in language that families and school staff can understand.
The EAPP plans to continue this project in 2025 to integrate the SF-AVS into workflows at Children’s Wisconsin cardiac clinics throughout the state and develop customizations for specialty cardiac conditions. The hope is to eventually create SF-AVS templates that can be used in other specialty clinics beyond cardiology. “It has been invaluable to work with a multidisciplinary, clinical team as we design and refine the school-friendly AVS, and I am so excited to see where the program has its greatest impact among our patients and families as we continue to roll it out,” said Christie Ruehl, JD, MBA, senior program manager of EAPP.
Project RECESS: Reimagining EAPP’s continuum of service for equity, effectiveness, efficiency, satisfaction & sustainability
Inspired by the SFHS framework, Project RECESS has helped the EAPP team shift from being a hands-on service provider to a limited number of families to supporting patients and families as an empowerment coach. The overall goal of Project RECESS is to improve program outcomes, efficiency and sustainability while helping parents and guardians become more self-sufficient in managing their child’s home, health and school care coordination.
One of the ways that the EAPP is helping empower families and encourage self-sufficiency is by providing easily accessible resources like a six-part “School Success Coaching” webinar series and one-on-one consult services. Since the shift in their approach, the EAPP has been receiving positive feedback from families. Post-webinar evaluations have shown a 95 percent overall satisfaction rate from families. The parent of a 4th grade student said: “I wish I would have been able to attend this years ago. For many years, I felt like I was drowning in this new world of special needs and medical complexities. Knowledge like this is very helpful for me.”
The EAPP received a new $250,000 grant from the Advancing a Healthier Wisconsin Endowment to continue this work for the next two years. With this funding, the EAPP team will continue its webinar series biannually focusing on:
- The parent as the project manager
- The link between health and learning
- Managing health at school
- Explaining the impact on learning
- Supporting education plans
- Planning for the future
“We are looking forward to building on our partnerships with schools and communities and sharing our model with other health systems,” said Cheryl Brosig, PhD, medical director of EAPP and chief of pediatric psychology and developmental medicine at Children’s Wisconsin. “The EAPP is seen as a leader in this work nationally, and other hospitals across the nation want to learn from us.”

Collaborating to improve Norwood outcomes
In 2023, the Herma Heart Institute decided to focus its efforts on a quality improvement project around the Norwood surgery, the first of three operations to treat hypoplastic left heart syndrome. Since the Norwood pathway was developed, outcomes improved significantly — and not just for the Norwood procedure.
“We intentionally chose a complex, high-risk patient group to focus on, believing that the insights could significantly impact other areas as well,” said David Saudek, MD, medical director for quality for the Herma Heart Institute.
The Herma Heart Institute typically performs 8 to 10 Norwood procedures a year.
“Children’s Wisconsin has always been a frontline leader for single ventricle palliation,” said Angelia Espinal, director of clinical outcomes at the Herma Heart Institute. “Over the last year, a multidisciplinary team has worked together to revamp our clinical pathway related to treating and caring for our Norwood patients, and we have made a lot of progress.”
The Norwood pathway team analyzed data from approximately 20 other institutions nationwide to determine best practices for every aspect of the operation and pre- and post-operative management. Then they discussed the granular details of their own practice and worked together to create a Standardized Clinical Assessment and Management Plan (SCAMP).
“All cardiac surgery is really a team sport,” said Michael Mitchell, MD, division chief of pediatric cardiothoracic surgery and co-surgical director of the Herma Heart Institute. “It requires a surgeon, anesthesia, perfusion, but also critical care, cardiology and our nursing teams and scrub technicians. So there are a lot of different individuals involved, and the Norwood is one example of a highly complex operation where small things make a huge difference.”
Since the team developed the new protocol, they’ve performed 10 Norwood surgeries. While it’s too early to gauge long-term outcomes, the Herma Heart Institute has cut the length of stay by half, as well as decreased the number of major adverse events. Survival rates are at the Society of Thoracic Surgeons’ median for survival.
The team continues to meet to discuss every Norwood case before and after surgery, refining their approach when necessary.
Meanwhile, outcomes for other heart surgeries are improving, too — adjusting narcotic use has had a positive effect on other cardiac patients’ length of stay.
Next, the team is working on applying this approach to a broader group of patients, including patients undergoing cardiac transplantation.
“Going through this process with our team has really moved the needle on all of our cases in a very dramatic way,” said Dr. Mitchell. “It’s been really profound to see.”
If you would like more information on our clinical pathways, please email hermaheartinstitute@childrenswi.org.

New clinical faculty
Children’s Wisconsin welcomes the following faculty members to the Herma Heart Institute

Bradley Johnson, MD, has joined our Adult Congenital Heart Disease (ACHD) Program as a cardiologist, after completing his ACHD fellowship at the Herma Heart Institute. He is also an assistant professor of cardiology at the Medical College of Wisconsin.

Osamah Aldoss, MD, comes to us from University of Iowa Stead Family Children’s Hospital. He is an interventional cardiologist, who has interest in transcatheter valves and working with ACHD patients. He is also a professor of pediatric cardiology at the Medical College of Wisconsin.
Graduated fellows
The Herma Heart Institute congratulates our graduated fellows

Felipe Murguia, MD, completed his fellowship in pediatric cardiology at the Herma Heart Institute and is now working on an advanced imaging fellowship at UT Southwestern.

Nicholas Rebhan, MD, completed his pediatric cardiology fellowship at the Herma Heart Institute and is currently in a fourth-year fellowship, focused on electrophysiology, at Vanderbilt University Medical Center.

Tracey Thompson, MD, completed her pediatric cardiology fellowship at the Herma Heart Institute and is currently pursuing advanced training in adult congenital heart disease.

Retired staff
The Herma Heart Institute congratulates these staff on their incredible careers. Their presence will be deeply missed but their legacies of innovation and compassionate care will endure.


Michele Frommelt, MD, retired from her 33-year career as a pediatric cardiologist at the Herma Heart Institute, as well as a professor of pediatric cardiology at the Medical College of Wisconsin. Over the last three decades, she has played a pivotal role in helping the Herma Heart Institute grow and evolve as a program — working to better understand treatment options for single ventricle patients, improving processes in the echo lab and establishing our fetal heart program. She has been known to go above and beyond to help patients and their families feel confident in understanding their diagnoses and trusting their medical decisions.

Maryanne Kessel, RN, MBA, retired after 37 years serving our patients and their families, first as a cardiothoracic nurse, then as the executive director of the Herma Heart Institute, and most recently, as the executive director of development for the Herma Heart Institute. In each of her roles, she has been masterful at connecting with patients and families and helping them navigate each chapter in their heart journey. She was pivotal in the strategic and fundraising efforts behind the Herma Heart Institute receiving its designation as an institute in 2017, which propelled the program’s focus on research and innovation. She has a special way of making each and every patient family feel supported, heard and comforted during some of their most challenging times.
We are so grateful to both Michele and Maryanne for dedicating their careers to the patients, families and staff of the Herma Heart Institute. They have both had tremendous impacts on our program and we are forever grateful for their guidance, support and friendship over the years.
Helping to shape the future of pediatric cardiology: The Herma Heart Institute hosts two conferences in 2024
This past year, the Herma Heart Institute was honored to host two prominent cardiac conferences in Milwaukee, Wis.
Robert Niebler, MD, leads a panel discussion at the International Conference on Pediatric Mechanical Circulatory Support Systems and Pediatric Cardiopulmonary Perfusion.
Robert Niebler, MD, leads a panel discussion at the International Conference on Pediatric Mechanical Circulatory Support Systems and Pediatric Cardiopulmonary Perfusion.
The first was the 18th International Conference on Pediatric Mechanical Circulatory Support Systems and Pediatric Cardiopulmonary Perfusion at the Pfister Hotel on May 9-10. Robert Niebler, MD, medical director of cardiac critical care at the Herma Heart Institute, co-chaired the event.
The meeting brought together clinical specialists in the fields of pediatric cardiology, cardiothoracic surgery, critical care and bioengineering to discuss research, clinical methods, groundbreaking developments and challenges in the field. Five countries, 17 states, and more than 35 different institutions were represented among the speakers and participants.
Molly Brickler, APNP, Michael Mitchell, MD, Robert Niebler, MD, and Alexander Raskin, MD, from the Herma Heart Institute, presented on a variety of topics.
Team members from the Herma Heart Institute, past and present, who attended the Midwest Pediatric Cardiology Society Annual Meeting.
Team members from the Herma Heart Institute, past and present, who attended the Midwest Pediatric Cardiology Society Annual Meeting.
Additionally, from Sept. 12-13, the Herma Heart Institute hosted the Midwest Pediatric Cardiology Society Annual Meeting at Saint Kate - The Arts Hotel. It was a record-setting conference with more than 160 attendees from 12 states and 22 institutions across the Midwest.
Attendees included physicians, nurses and medical staff who care for patients in the pediatric or adult congenital heart disease populations. The group came together to explore and collaborate on new research and quality improvement initiatives happening throughout the Midwest. Many staff from the Herma Heart Institute gave presentations or presented on a poster.
The Herma Heart Institute is proud to have supported both of these conferences and highlighted the important contributions that our team has made to help advance the field of pediatric and adult congenital cardiology.

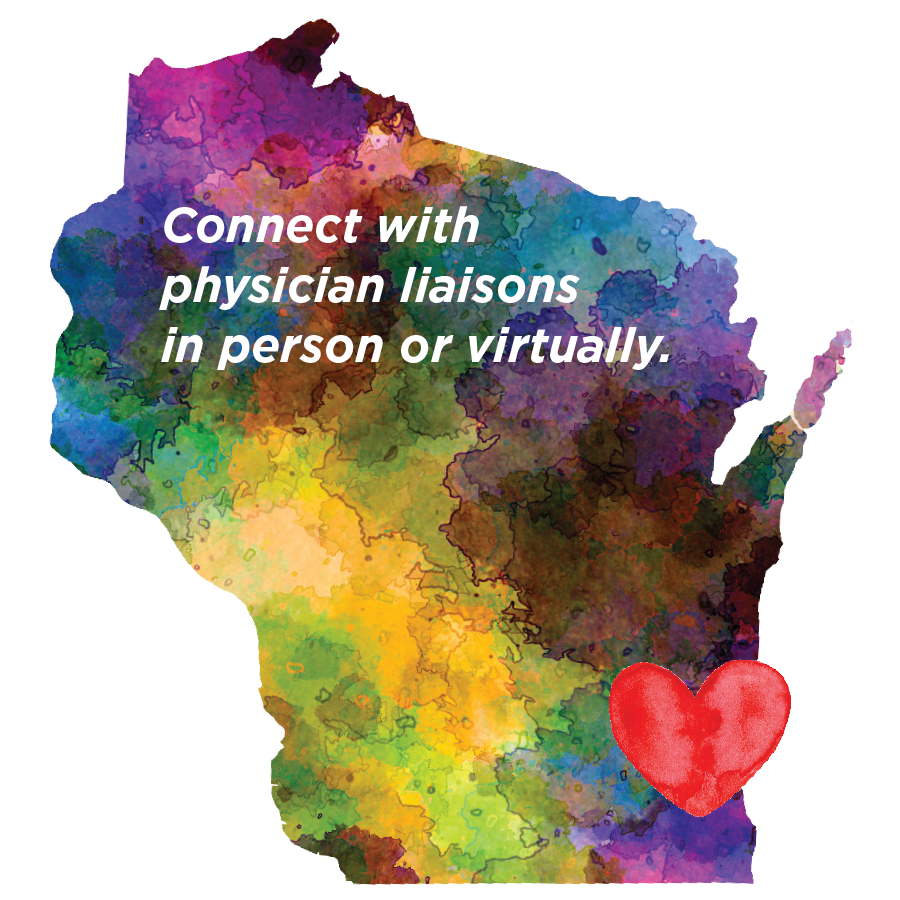
Here for you whenever or wherever you need us
The Children's Wisconsin physician liaison team is dedicated to developing and maintaining relationships with referring physicians.
In addition to serving as a link between Children's and
referring physicians, your liaisons can:
- Provide information about Children's services and programs
- Direct you to continuing education opportunities
- Facilitate solutions to referral issues
Contact your liaison:
|
Metro Milwaukee |
Southeast Wisconsin |
Northeast Wisconsin |
|
Lisa Magurany |
Margie Berg (414) 336-1342 mberg2@childrenswi.org |
Diane Dorow (920) 982-5613 ddorow@childrenswi.org |
Outside a physician liaison territory:
Physician Support Services
(414) 266-2310