Message from the In-Chiefs
Children’s Wisconsin began as a volunteer hospital founded by a group of women who recognized there needed to be a place for kids to receive medical care. It began in a house in what is now downtown Milwaukee. Over time it grew, largely due to the beneficence of the citizens of Milwaukee and the growing recognition that children have medical and social needs that are best addressed by a special place for child health care.
Making Wisconsin's children the healthiest in the nation
Together, Children’s Wisconsin and our academic partner, the Medical College of Wisconsin, are united to carry that concept forward. Our vision is that children in Wisconsin should be the healthiest in the nation. To accomplish that, the diagnostic, anesthesia and surgical health teams have set our focus on what is best for kids. This translates to having the best pediatric specialists using the best technologies designed for kids, applied with the best scientific principles, in an environment rich in resources dedicated to caring for children.
One way that we marshal those resources is through our multidisciplinary clinics. For children with complex conditions, rather than have them travel to several specialists, we bring all the providers together to hear how their disease will be managed. This type of care is very patient-focused. It is resource-intensive for us but leads to better outcomes for the child.
We also are committed to bringing new, evidence-based treatments to the children we care for. One such treatment you will read about is a minimally invasive surgical approach to chest wall conditions, which can potentially shorten recovery time. We will also be reporting on a new cryoablation technique that addresses postoperative pain associated with pectus surgery.
In alignment with our core value of ensuring that we are providing the best and safest care for children, our nurses and technologists are dedicated to providing care exclusively for children. Additionally, every provider and staff member in our imaging department is completely focused on the care of children, and our radiologists are all subspecialty trained as pediatric radiologists. This makes a difference because our faculty has also pursued additional subspecialties, such as pediatric vascular interventional radiology or pediatric neuroradiology.
The pediatric specialists at Children’s Wisconsin are highly skilled at communicating with kids and family members. Beyond the exceptional medical care that our anesthesiologists, radiologists, surgeons and nurses provide, we also rely on resources like pediatric mental health and the Child Life and Creative Arts Therapies program to help address the emotional health needs of children receiving care at Children’s Wisconsin. Whether a child needs care for two hours, two weeks or two months, we offer play therapy, educational services and simple things like video games and movies. This helps make Children’s Wisconsin a more comfortable and welcoming environment for a child in need of care that any of us would find anxiety-provoking, let alone a young child.
As you review this report, please know we share your commitment and dedication to young patients. We are here to help you bring them the best possible care.
Our surgical team comprises our newest surgeon, Tracy Geoffrion, MD (right); our division chief, Michael Mitchell, MD (center); and our director of heart transplantation, Ronald Woods, MD, PhD (left).
Our surgical team comprises our newest surgeon, Tracy Geoffrion, MD (right); our division chief, Michael Mitchell, MD (center); and our director of heart transplantation, Ronald Woods, MD, PhD (left).
A legacy of innovation in pediatric heart care
How cardiothoracic surgery at Children’s Wisconsin embraces advanced technology for complex procedures
For more than 65 years, the Herma Heart Institute at Children’s Wisconsin has maintained a legacy of pediatric heart care breakthroughs. As we look toward the future, we will never stop working in our quest to make the sickest children well again. This legacy of challenging paradigms of care and improving outcomes is embraced by our current cardiac surgical team. We continue to strive to improve the care we can deliver and break new ground using innovative surgical and scientific technology.
Teamwork, transparency and innovation
Our surgical team comprises our newest surgeon, Tracy Geoffrion, MD; our director of heart transplantation, Ronald Woods, MD, PhD; and our division chief, Michael Mitchell, MD. Together, we are committed to achieving the best possible outcomes for all patients in our program by working toward consistent and reproducible results and by innovating in cases that require modifications and creative solutions. We apply transparency in reporting and quantitative analysis to refine our techniques and performance. Programwide, we are embarking on efforts to reduce morbidity and mortality and also minimize minor complications, residual lesions and length of stay.
Many cases that we encounter fall outside of the typical, and our service is seeing an increase in the percentage of STAT 3, STAT 4 and STAT 5 cases, which represent the more complicated cases in our specialty. In addition, we see many cases that fall outside of the benchmark labels, and several that are profoundly high risk sent in from outside our region. It is in some of these cases that particularly innovative approaches to care are required.
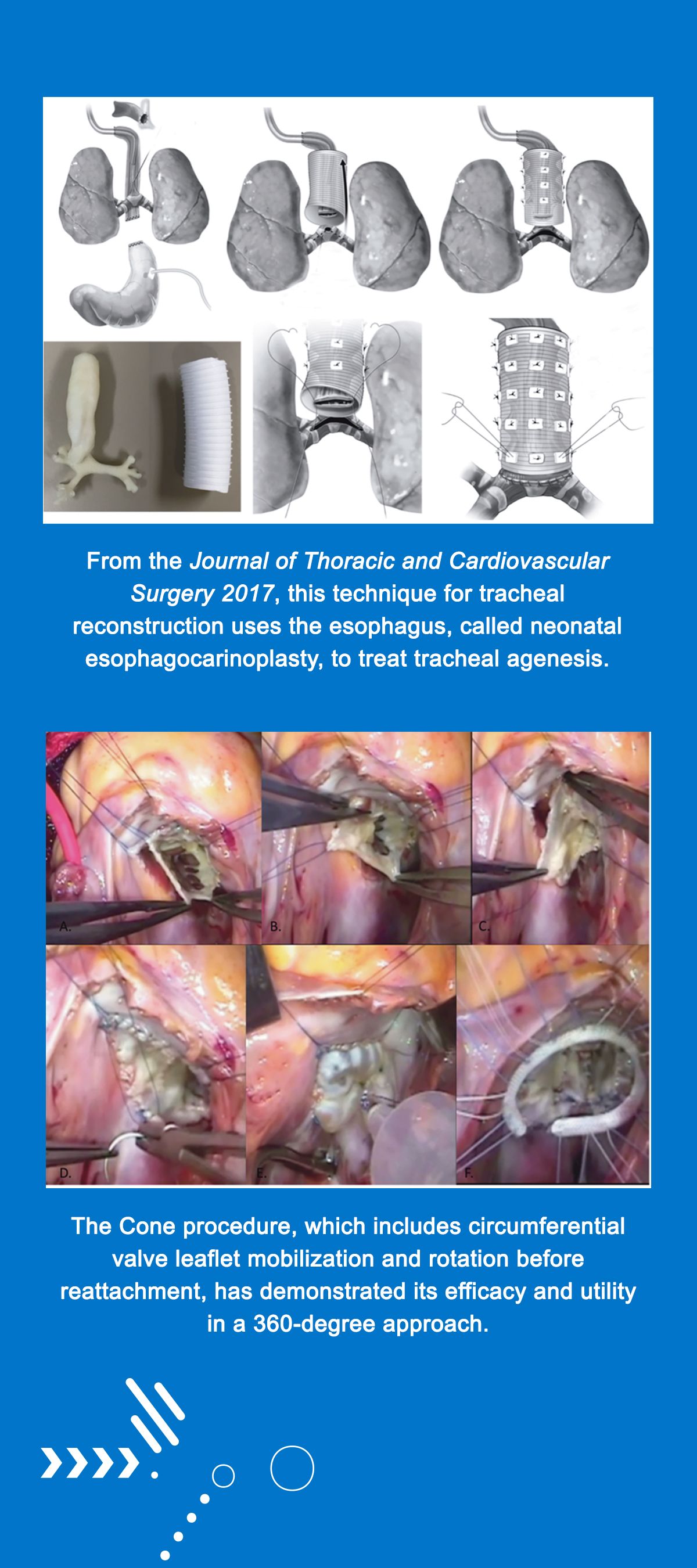
Recent surgical innovations from our team that have been applied in patient care include development and utilization of the 360-degree modification of the Cone procedure. This involves a circumferential mobilization of the valve leaflets and rotation prior to reattachment and has proven useful in reconstruction of some of the most severe variants of Ebstein’s anomaly. This work was reported in the Annals of Thoracic Surgery and presented at the Society of Thoracic Surgeons. It continues to be utilized successfully in patients at Children’s Wisconsin as well as in Lima, Peru.
Our program is increasingly faced with complex single-ventricle patients who, although successfully palliated through the Fontan circulation, are presenting in severe heart failure, sometimes refractory to medical management. Some of these cases require mechanical circulatory support, often with creative ventricular assist device strategies to bridge the patient to successful heart transplantation. Our team has pioneered a modified total artificial heart support technique in which the cardiac mass is removed and valved conduits and existing cannulas are configured to create a biventricular in series circulation. Although this work carries extreme risk, we have had success in supporting several patients who were otherwise unsalvageable then were able to make it through successful heart transplantation.
The Herma Heart Institute has an active clinical and research cord blood bank, which allows for development and future personalized stem cell therapeutics. We are collaborating with basic and translational scientists within our program, and have generated published innovations on the pathway to development of personalized biological beating patches for staged surgical reconstruction to be used from the neonatal period through adulthood.
Finally, our team has led the field in developing and successfully applying a technique for tracheal reconstruction using the esophagus, called neonatal esophagocarinoplasty, to treat a previously almost uniformly fatal condition, tracheal agenesis. This technique has been applied to three neonates and infants with two long-term survivors.
Continuous improvement
The high standard of innovation that our surgical team brings to the operating room requires the hard work and contribution of all members of our extended surgical team, including our perfusionists, physician assistants, nurse clinicians, cardiac anesthesiologists, critical care specialists and cardiologists, as well as close collaboration with other departments including neonatology, ENT, pulmonology and general surgery.
We are driven by the desire to improve outcomes for all patients. We know we have considerable work ahead. We believe progress is made by stepwise improvement in processes with quantitative metrics measuring each advance, as well as by major conceptual leaps forward for the most complicated patients. Innovation often arises from necessity. Once innovation occurs, our measure of success is that it can be effectively and repeatedly applied. We are motivated by this challenge and the opportunity to continue to improve outcomes for our patients.
Nasoalveolar molding aids in cleft lip and palate repair
The craniofacial orthodontic program at Children’s Wisconsin demonstrates collaborative care with the plastic surgery and cleft lip and palate team
Jameson in July 2023, following 17 NAM visits and one month after his lip repair surgery. He will continue receiving his treatment and care with our cleft lip and palate team into adulthood.
Jameson in July 2023, following 17 NAM visits and one month after his lip repair surgery. He will continue receiving his treatment and care with our cleft lip and palate team into adulthood.
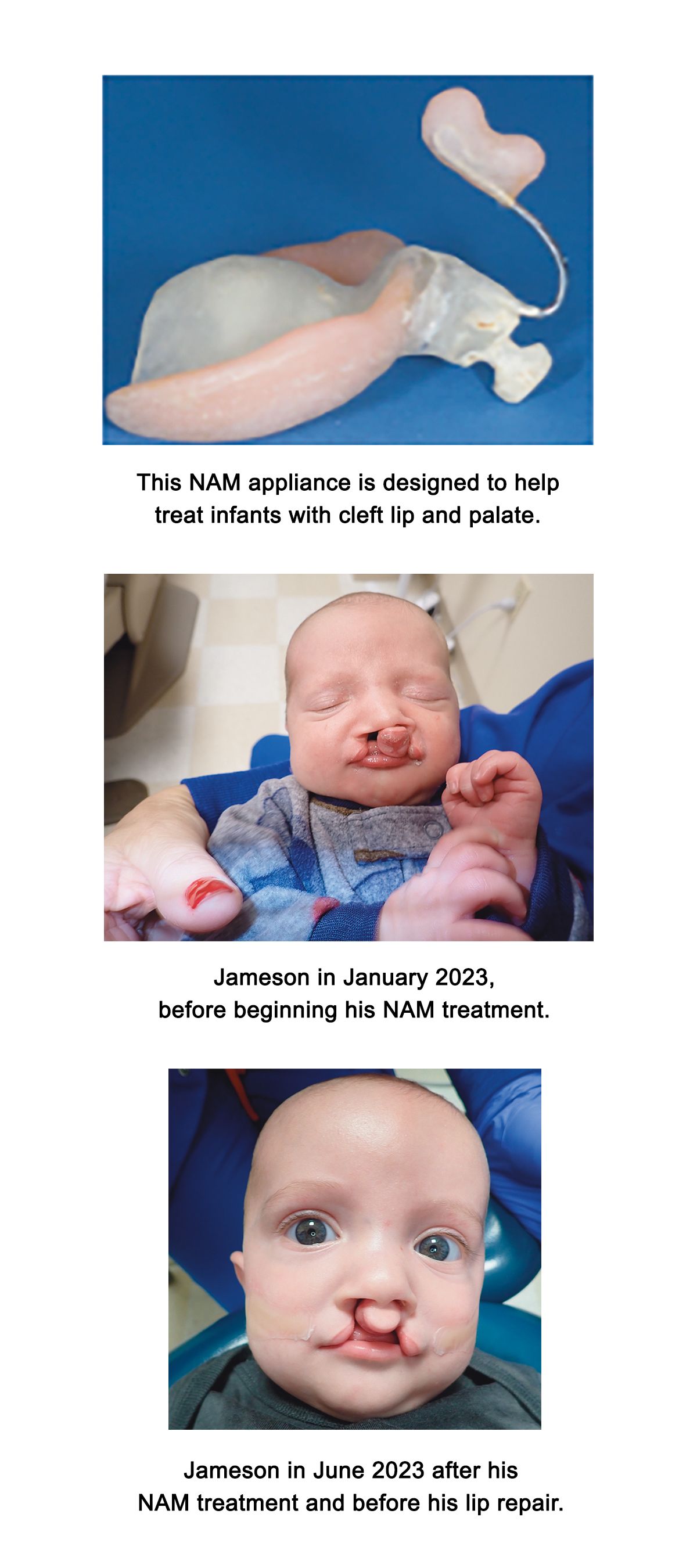
Cleft lip and cleft palate are among the most common congenital facial differences seen at birth, with various presentations of the conditions occurring in approximately 1 in every 700 births in the United States. The upper lip and palate form during embryogenesis around six to eight weeks. Failures to fuse these facial processes result in a cleft lip and/or palate. This may happen spontaneously or be attributed to genetics, particularly if the cleft is related to a syndrome. Risk factors for orofacial clefting include maternal smoking, diabetes, folate deficiency and using certain medications to treat epilepsy, such as topiramate or benzodiazepines, during pregnancy.
Ultrasound imaging may detect a cleft during the second or third trimester. The cleft lip and palate team, which is part of the Plastic Surgery Program at Children’s Wisconsin, offers prenatal visits to help guide families for their child’s arrival. On delivery, the provider examines the child’s cleft, respiration, feeding and hearing to determine possible associations of syndromes characterized by cleft lip and/or palate. Infants presenting without a syndrome typically do not have higher rates of birth complications. Soon after, the family meets the child’s pediatric reconstructive plastic surgeon. The surgeon provides options to help prepare the child for lip repair, including nasoalveolar molding (NAM) therapy.
How NAM therapy works
NAM therapy began in New York in the 1980s with Barry H. Grayson, DDS, and Court Cutting, MD. Pamela Hanson, DDS, trained with Dr. Grayson and embedded this care into Children’s Wisconsin in the early 1990s. Today, more than 30 percent of cleft and craniofacial teams in North America provide NAM, and its use is increasing in frequency. NAM is a presurgical therapy used to reduce the size of the cleft lip and alveolus, lengthen the columella and shape the nose on the cleft side to help improve the results of the lip repair.
NAM begins within the first few weeks of life with the average treatment time of three to six months, followed by the child’s lip surgery. In the hospital setting, the orthodontist takes an intraoral impression of the maxilla to fabricate the appliance out of acrylic. It rests on the palate, similar to an orthodontic retainer. Taping is used with the appliance to help bring the segments closer together and for retention. Nasal stents are added later to help shape the nose as the segments come together. Weekly visits occur with the orthodontist to evaluate progress and adjust the appliance. The child wears the appliance all day, including while feeding and sleeping, and parents refresh the adhesive strip tapes and clean the appliance daily.
What NAM therapy entails for patients
The initial burdens of care are considerable, including increased visits, traveling, home management, temporary cheek or gum irritations and initial financial costs. However, appropriate use, compliance and technique with NAM are effective in the preoperative closure of the cleft and in improving nasal aesthetics. In the long term, evidence suggests fewer revision surgeries are needed, offsetting the additional financial burden and minimal adverse impacts on facial growth. Additionally, studies show that parents participating in NAM reflect reduced depression and anxiety during treatment.
Dr. Hanson, orthodontist, and Cleo Yi, DMD, craniofacial orthodontist, have more than 30 years of combined experience providing NAM care for families. Here’s the story of one family’s experience with NAM.
Jameson’s family began their partnership with the cleft lip and palate team at Children’s Wisconsin during prenatal consultations and were introduced to NAM therapy. Only 11 days after Jameson was born, his parents brought him in to see Dr. Yi for a consultation for NAM therapy. Within a couple of weeks, the NAM appliance was made and fitted for Jameson, and he began wearing it full time.
His parents persevered through the initial learning curve of managing the appliance at home and continued to visit Children’s Wisconsin weekly for adjustments to the appliance. The parents make this treatment work. Jameson and his parents worked hard to ensure he wore the appliance correctly and safely at home. Though Jameson grew to be a magician, taking out his appliance independently toward the end, Jameson and his family did an amazing job. In late spring of this year, Jameson and his family celebrated their accomplishments with his NAM “graduation” before his lip repair just a few days later. Jameson will continue receiving his care with our cleft lip and palate team into adulthood.
“We’re grateful to the families and providers with the Children’s Wisconsin cleft lip and palate team, and believe each smile has such professional and personal meaning. It is an honor to journey with these families through their child’s growth.”
Cleo Yi, DMD, Craniofacial Orthodontist, Children's Wisconsin
Cleo Yi, DMD, Craniofacial Orthodontist, Children's Wisconsin
A look at the chest wall program at Children’s Wisconsin
Treating chest wall changes at Children’s Wisconsin addresses multiple physical and mental aspects for older children
John C. Densmore, MD, Pediatric General and Thoracic Surgeon, Children's Wisconsin; Professor of Pediatric General and Thoracic Surgery, Medical College of Wisconsin
John C. Densmore, MD, Pediatric General and Thoracic Surgeon, Children's Wisconsin; Professor of Pediatric General and Thoracic Surgery, Medical College of Wisconsin
Take a moment and put yourself back in your shoes as a teenager. You were beginning to form your ideas of the world around you and how you relate to it. The existential question often at the center — what is my purpose in this life? — is met with myriad activities, newfound friendships, external expectations and a yearning for independence.
Now add a slow but undeniably persistent change in your chest wall to this hormonal and energetic time. In your case, it is a constant reminder of how different you are from your peers. As you catch the sight of yourself in the mirror, you are continually dismayed as the center of your chest sinks progressively deeper. You wonder how noticeable it is to your friends and where your heart and lungs find room to keep you going. Why did this happen to me? How will dating go? Can I be the athlete that I want to be?
These doubts and fears are kept deep and hidden by a stoic front as you work to pursue your dreams. But pragmatically, there is a preference to keep hidden behind shirts, swim shirts, towels and doors. You cast aside worrisome thoughts of limitation when they enter your head, but they are there. Your parents are worried too and may feel responsible, but this is your blueprint and your life to live.
Improving patient outcomes with multidisciplinary care
Most parents would agree that a progressive deformity occurring during these formative years and the associated psychosocial effects present more than a cosmetic problem. At Children’s Wisconsin, we have worked to understand and help patients and families affected by chest wall abnormalities like pectus excavatum, pectus carinatum, slipping rib syndrome and postpneumonectomy syndrome. We have met these families with multidisciplinary expertise, including inpatient and outpatient nursing, physical and occupational therapy, pharmacy, psychology, pain medicine and administrative coordination. The ethos of this working group is to fully and safely meet the needs of our patients and families confronted with worrisome and abrupt chest wall changes.
Our surgical approach shifted in 1999 after a visit from Don Nuss, MD, innovator of the minimally invasive repair of pectus excavatum, where he completed the first Nuss procedure at Children’s Wisconsin. The sternum is immediately forced into a new position using a U-shaped bar made of stainless steel that is a quarter of an inch thick and spans the chest. Persistent postoperative dull bony pain was seen to subside one month later. As postoperative pain management became the early recognized challenge for recovery, the Nuss Working Group emerged. Organically assembled in 2016 with a common interest in improving patient outcomes, this group guided the transition from epidural catheters to a multimodal pain strategy based on patient-controlled analgesia.
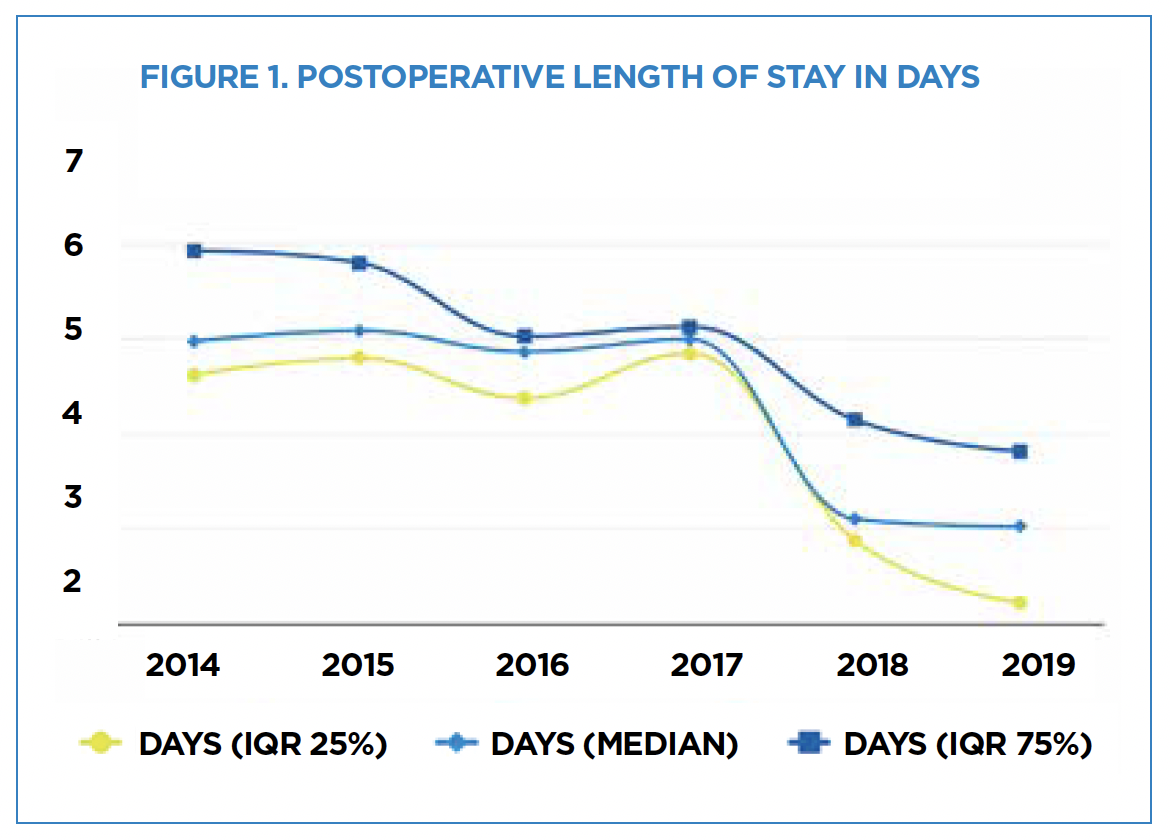
With this group’s ongoing effort, patients saw progressive decreases in length of stay from 5.2 days to 2.5 days (Figure 1) and a 50 percent reduction in inpatient and outpatient opioid dosing. Surgeons and patients have also reported an improved patient experience. In the last two years, intraoperative cryoanalgesia has become standard, resulting in an average stay of 1.6 days. Many of our cryoanalgesia patients are currently managed without postoperative narcotics. The change in recovery in the last five years has been markedly improved and is moving the Nuss procedure toward day surgery.
Continuing to advance care
While shifting to cryoanalgesia may seem to prevent the need for a multimodal pain strategy, the lessons learned are still essential for our skeletally mature patients (more than 18 years old) with greater postoperative pain needs. A continuing benefit discovered in the multimodal pain strategy is routine psychologic care. Our team works to identify those who will most benefit from surgical intervention, provides coping skills and addresses unmet mental health needs in preparation for surgery.
Our group has iterated more than 10 pathways for our chest wall surgery patients as techniques evolve. These pathways include the preoperative evaluation (pectus-protocol cardiac-gated MRI) and postoperative recovery. Among the nearly 600 Nuss procedures completed since 1999, our patients have avoided cardiac injury and experienced complication rates lower than the national average. Our select pediatric surgeons work to align practice and techniques, often assisting one another alongside our highly skilled pediatric surgery fellows and physician assistants to achieve the most optimal surgical correction. A long list of postoperative families volunteer their surgical experience with families coming to terms with chest wall changes.
We have applied these lessons broadly to other chest wall conditions, and continue to innovate and adopt new techniques as evidence and intuition guide us. Examples include using Klobe Bell for preteens with pectus excavatum, compressive brace therapy for pectus carinatum and partial Ravitch approaches for mixed chest wall changes. We continue this work joyfully and keep the following question in mind when providing care: What would we want for ourselves or our children when faced with a chest wall change?

Epilepsy practice grows with new epileptologists, procedures and clinics
How Children’s Wisconsin is investing in all three to bring the best pediatric epilepsy care to the state
It’s an exciting time for the Epilepsy Center at Children’s Wisconsin. The surgery team within the Epilepsy Center was impacted when key epileptologists departed in 2019, as well as from the effects brought on by the COVID-19 pandemic. With strong support from Children’s Wisconsin, Matthew Harmelink, MD, chief of pediatric neurology, successfully recruited four pediatric epileptologists who have helped rebuild our program.
Sean Lew, MD, Medical Director of Pediatric Neurosurgery, Children's Wisconsin; Chief and Professor of Pediatric Neurosurgery, Medical College of Wisconsin
Sean Lew, MD, Medical Director of Pediatric Neurosurgery, Children's Wisconsin; Chief and Professor of Pediatric Neurosurgery, Medical College of Wisconsin
Rene Andrade-Machado, MD, PhD, is a fellowship-trained pediatric epileptologist in neurophysiology and came to Children’s Wisconsin from Detroit Medical Center. There, he furthered his formal training in pediatric epilepsy, having previously developed and led an epilepsy program in Colombia.
Pradeep Javarayee, MD, is associate director of pediatric epilepsy and received his training at Cincinnati Children’s in child neurology and pediatric epilepsy before holding a faculty position at the University of Louisville.
Avantika Singh, MD, received her pediatric training at the Medical College of Wisconsin, then obtained her child neurology and epilepsy training at Boston Children’s before returning to Milwaukee. She specializes in early developmental epilepsy from birth through 2 years old.
Elham Abushanab, MD, received her training in child neurology and epilepsy at the Cleveland Clinic. She has a special interest in the genetics of epilepsy.
The epilepsy surgery program is stronger now than it has ever been. As of September 2023, we have already exceeded the surgical volume of our prior peak in 2018. The epilepsy program has continued to innovate and expand our offerings to provide children with the best possible epilepsy care. Some examples of this include:
Magnetic resonance imaging-guided stereotactic laser ablation: This procedure involves inhibiting the bihemispheric spread of epileptic activity by partially or entirely sectioning the corpus callosum, the main highway of communication between the two halves of the brain. It has traditionally been performed as an open craniotomy, but we can now offer a minimally invasive technique involving four 5-mm incisions, with less postoperative pain and scarring. We recently published a technique paper reporting on three patients undergoing a complete corpus callosotomy with this technique.
Responsive neurostimulation: This therapy is reserved for patients whose seizures are uncontrolled by medication but are not good candidates for traditional resective or ablative surgery due to the functional importance of the brain involved with seizure onset or due to seizures emanating from multiple bilateral areas of the brain. A responsive neurostimulator device monitors brain activity through the help of electrodes implanted in specific regions of the brain.
If the electrodes detect seizure activity, they immediately provide electrical stimulation to the area of the brain to disrupt the seizure. This procedure is typically used only on patients 18 years and older, but it has been successful at Children’s Wisconsin for an 8-year-old girl. After the procedure, her seizures dropped from about once a week to once a month or even less frequently. The family has not had to use rescue medication since the neurostimulator was implanted.
Endoscopic-assisted hemispherectomy: This is a less invasive form of hemispherectomy, which involves a pure disconnection rather than resection of one hemisphere of the brain responsible for causing seizures. Hemispherectomy is usually performed as a combination of brain removal and disconnection with a larger incision and opening in the skull. The less invasive approach allows for less postoperative discomfort, scarring and blood loss.
Magnetoencephalography: The epilepsy centers at Children’s Wisconsin and Froedtert & the Medical College of Wisconsin remain the only ones in the state to offer magnetoencephalography. This noninvasive test measures the magnetic fields produced by the brain’s electrical currents, enabling us to map brain function and identify likely sources of epileptic activity, aiding in surgical planning.
Expanding access with a focus on the youngest epilepsy patients: It has long been known that children with intractable epilepsy benefit from earlier surgical intervention, both in terms of seizure resolution as well as long-term cognitive development. Thus, it is exciting that Dr. Singh has launched a new clinic focused on early developmental epilepsy that will enable us to identify and intervene earlier in these children and lower the chance of curable epilepsies taking an unnecessary toll on children’s developmental potential.
Taking the right approach: Our epilepsy program is a close collaboration between multiple specialties, including neuroradiology, neuropsychology, neurology and neurosurgery. We’re excited to announce that we are expanding our neurology and epilepsy care to Northeast Wisconsin. Our growing expertise and capacity will allow us to consider more patients for surgical options. Our multidisciplinary approach and advanced surgical techniques help reduce seizures and improve the quality of life for children with severe and medically challenging cases of epilepsy.
Training the next generation of pediatric eye care providers
Why quality eye care takes a multidisciplinary team and how Children’s Wisconsin is building one
When I joined Children’s Wisconsin and the Medical College of Wisconsin (MCW) in 2015, the division had just one pediatric ophthalmology clinic location with four exam lanes, two full-time pediatric ophthalmologists, one pediatric optometrist and 1.5 orthoptists. The wait for a new patient appointment was eight months.
One major challenge was the low number of ophthalmology specialists entering pediatrics. We realized that if we were to continue to grow, we needed to expand our provider workforce. Since then, the department has developed strategically through recruitment and pioneering new training pathways.
Alex Khammar, MD, Medical Director, Pediatric Ophthalmology, Children's Wisconsin; Associate Professor, Medical College of Wisconsin
Alex Khammar, MD, Medical Director, Pediatric Ophthalmology, Children's Wisconsin; Associate Professor, Medical College of Wisconsin
Providing mentorship from the beginning
We offer first- and second-year MCW medical students shadowing opportunities in our clinic. We also offer an elective in ophthalmology to third-year students that includes pediatric ophthalmology and a fourth-year ophthalmology sub-internship specific to pediatric ophthalmology. At the resident level, we mentor ophthalmology residents and serve as clinical research advisors to educate and excite them about pediatric ophthalmology.
We established a pediatric ophthalmology fellowship program and graduated one person who joined our team. Several pediatric ophthalmology fellowship programs in the country go unfilled each year, and the profession is facing a crisis as fewer ophthalmology residents choose to specialize in pediatrics.
Growing interest in pediatric optometry
There is a similar shortage of pediatric optometrists. Given the growing interest nationally to have pediatric optometrists train and work in hospital-based programs, we partnered with MCW to launch a one-year pediatric optometry residency. Of the 36 pediatric optometry training programs in the country, only eight, including ours, are hospital-based.
Our program has become highly competitive given the value that well-trained, hospital-based pediatric optometrists bring to a service and their ability to extend the breadth and number of patients that can be seen. We’ve had three graduates so far. One recently started seeing patients full time at the new Children’s Wisconsin Appleton Clinic.
Leaders in orthoptic education
Orthoptics is a profession whose primary emphasis is the diagnosis and non-surgical management of strabismus, amblyopia and eye movement disorders. They play a critical role in both pediatric and adult eye care. We have one of the most extensive orthoptic programs in the country. Children’s Wisconsin is also home to 1 of 16 orthoptic training programs. Our goal is to serve not just our own community but to develop a training program that is a national leader in orthoptic education. To date, we have graduated two orthoptists, both of whom we’ve hired. We have two students in the program, including former technicians advancing to orthoptics. Our students have presented at national meetings and other institutions, including Johns Hopkins and the University of Oregon.
There is also a national shortage of pediatric eye care technicians. This inspired us to start a technician-in-training program to create a pipeline for our pediatric workforce and improve the availability of specialized technicians.
Tailoring care to those we serve
Our efforts have paid off. Today, we have four clinic locations within Southeast Wisconsin and the Fox Valley with 28 exam lanes (expanding to 32 by 2025). Six pediatric ophthalmologists, four pediatric optometrists, eight orthoptists and other support staff provide robust regional care. We also subspecialize in areas like retinopathy of prematurity and adult strabismus, allowing more complex care to be delivered locally and, in August 2023, became an ocular oncology destination service.
At Children’s Wisconsin, we provide photographic diabetic eye screenings the same day as endocrinology clinic visits to increase screening volumes, provide orthoptist support to the MCW Department of Ophthalmology and Visual Sciences for neuro-ophthalmology and complex adult strabismus patients and support several hospitals in the region in preventing, diagnosing and managing retinopathy of prematurity.
Our work continues. We are seeking opportunities to continue collaboration with our academic partners to create novel pipelines to provide pediatric eye care. We also plan to expand our current training programs to offer additional opportunities for our team members to “grow in place” in their professional development.
We started these programs because hope was not a strategy for building our workforce. We couldn’t rely on other institutions to produce these specialists because they weren’t available. These training programs were born out of necessity to care for the population we serve.
Our efforts to increase the number of pediatric eye care practitioners at multiple levels is one of the most purposeful and effective achievements we’ve made in recent years. I look forward to seeing our efforts grow and our graduates join our team or the teams of other pediatric ophthalmology programs nationwide.
Going beyond ear tubes
and tonsils
How the Children’s Wisconsin Otolaryngology Program is working with others to innovate multidisciplinary programs
Our team of board-certified complex pediatric otolaryngologists knows that the field goes beyond the ear, nose and throat. Otolaryngologists also perform a diverse range of procedures, including mass removal in the head and neck, upper and lower airway procedures to help improve breathing, sinus surgeries and foreign body removal from the ear, nose, airway and swallowing passages.
Cecille G. Sulman, MD, Medical Director of Pediatric Otolaryngology, Children's Wisconsin; Chief and Professor of Pediatric Otolaryngology, Medical College of Wisconsin
Cecille G. Sulman, MD, Medical Director of Pediatric Otolaryngology, Children's Wisconsin; Chief and Professor of Pediatric Otolaryngology, Medical College of Wisconsin
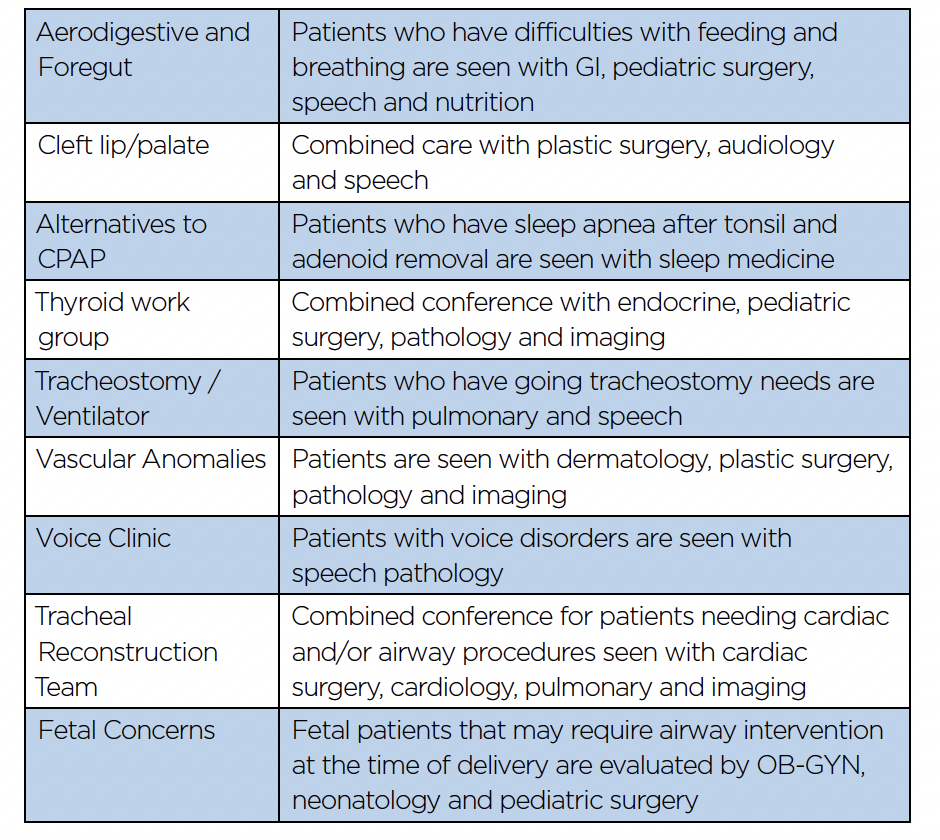
Being a comprehensive service line also means working with other departments to stay innovative. Learning where we intersect with other services to assist children with complex care needs is how the Otolaryngology Program stays on top of advanced care. Each day, the otolaryngology specialists at Children’s Wisconsin partner with our colleagues in audiology, speech and language pathology to ensure our patients receive timely and effective care for various disorders affecting hearing and communication. This high level of care will help these children develop and improve language skills.
Many dedicated multidisciplinary programs at Children’s Wisconsin exist to streamline care, improve communication among specialists and reduce the need for excessive visits. We are proud to work with our colleagues in various specialty clinics (Table 1).
Table 1. Multidisciplinary teams that include pediatric otolaryngology
Table 1. Multidisciplinary teams that include pediatric otolaryngology
Airway management is a team effort
For children who cannot support their breathing without a ventilator due to prematurity or a narrow airway, a common procedure is placing a tracheostomy tube in the neck to allow them to breathe and be cared for at home. The best part about caring for a child with tracheostomy tubes is getting them to the point where they can be removed.
Working collaboratively with our colleagues on the pulmonary and respiratory therapy teams in the tracheostomy and home ventilator program, our providers help guide this process for safe airway management. Another vital part of our program is the tracheal reconstruction team, which focuses on children with heart and breathing problems. With the assistance of cardiac surgeons and pulmonologists, we coordinate procedures to improve breathing that may involve airway evaluation and open chest procedures.
Otolaryngology care begins before birth
At the Children’s Wisconsin Fetal Concerns Center, a fetus may be identified with a mass or structural problem that could possibly interfere with breathing upon delivery. In addition to obstetrics, gynecology, pediatric surgery and neonatology, we consult with families to help them best manage their child’s breathing from birth. This may involve a pediatric otolaryngologist intervening or establishing an airway at the delivery. At the same time, the infant is still connected to the mother by the umbilical cord, known as an ex utero intrapartum treatment — or EXIT procedure.
This complex procedure is available at only the most specialized centers, and the Fetal Concerns Center at Children’s Wisconsin performed the state’s first EXIT delivery in 2010. We continue to work with our teams to carry out this procedure and help babies with airways obstructed by tumors or other fetal anomalies, such as congenital diaphragmatic hernia or congenital pulmonary airway malformation.
Treating sleep conditions
Our department also treats obstructive airways through the alternatives to the CPAP program. Some children who had their tonsils and adenoids removed may experience persistent airway blockage. This may be the case in children with conditions such as Down syndrome or obesity. In addition to medical therapy recommendations from sleep medicine, we offer sedated endoscopy to check for blockage sites and perform additional sleep surgical procedures if indicated to address the obstructing parts of the child’s airway.
Children’s Wisconsin will soon offer a new procedure called the Inspire device. This device is meant for children 13 years and older with Down syndrome who suffer from sleep apnea. Since the FDA has granted expanded approval to the Inspire neurostimulation device to treat pediatric patients with Down syndrome who have obstructive sleep apnea, we can also broaden pediatric care to those who cannot be effectively treated with continuous positive airway pressure therapy.
Otolaryngology care continues to expand
Additional areas of innovation include the voice clinic, in which patients with voice disorders are evaluated with speech therapy. We offer a cutting-edge surgery to treat patients with a paralyzed vocal fold and poor speech called reinnervation of the recurrent laryngeal nerve, which stimulates voice box movement. Similarly, the vascular anomalies program has partnered with colleagues in dermatology, plastic surgery and interventional radiology to remain at the forefront of innovative care for children with blood vessel and lymphatic malformations. The team is known for the discovery of a new use of a medicine known as propranolol in treating hemangiomas.
Our physicians are supported by an excellent team of advanced practice providers who participate in numerous multidisciplinary programs. They are highly trained to support the patients in care coordination and ongoing patient care. With a team of nine physicians and nine APPs, the pediatric otolaryngology program at Children’s Wisconsin is here to help patients with routine health needs and collaborate with specialty teams to provide the best care for children.

The multidisciplinary world of pediatric plastic surgery
A closer look at three multidisciplinary clinics where plastic surgery plays a significant role at Children’s Wisconsin
Pediatric plastic surgeons have a long tradition of working collaboratively with many other specialties to care for patients with complex medical conditions. Organized multidisciplinary clinics (MDCs) provide comprehensive, coordinated care across many organ systems. MDCs also facilitate patient and family attendance by offering convenient access to multiple specialties in one location and at one time.
We want to highlight three MDCs at Children’s Wisconsin where plastic surgery plays a central role in caring for patients with craniofacial deformities, including two new clinics unique to Children’s Wisconsin and not found elsewhere in Wisconsin.
(Left to right) Kristen Klement, MD, Pediatric Plastic Surgeon, Children’s Wisconsin; Associate Professor of Pediatric Surgery, Medical College of Wisconsin; Sameer Shakir, MD, Pediatric Plastic Surgeon, Children’s Wisconsin; Assistant Professor of Pediatric Plastic Surgery, Medical College of Wisconsin; Kant Lin, MD, MBA, Medical Director of Plastics and Reconstructive Surgery, Children’s Wisconsin; Chief and Professor of Pediatric Plastic Surgery, Medical College of Wisconsin
(Left to right) Kristen Klement, MD, Pediatric Plastic Surgeon, Children’s Wisconsin; Associate Professor of Pediatric Surgery, Medical College of Wisconsin; Sameer Shakir, MD, Pediatric Plastic Surgeon, Children’s Wisconsin; Assistant Professor of Pediatric Plastic Surgery, Medical College of Wisconsin; Kant Lin, MD, MBA, Medical Director of Plastics and Reconstructive Surgery, Children’s Wisconsin; Chief and Professor of Pediatric Plastic Surgery, Medical College of Wisconsin
Cleft lip and palate clinic
Cleft lip and/or cleft palate are among the most common congenital anomalies, with an incidence of about 1 in 700 live births (including the dental intervention treatment described on p. 6). Treatment begins prenatally with providing guidance and support to expecting parents. This care continues throughout childhood at our MDC. Our clinic, which has been approved by the American Cleft Palate Craniofacial Association, allows children to see multiple providers in one visit. Plastic surgery orchestrates the team, but comprehensive care of the child occurs with other specialties’ help.
Speech therapy is critical after birth to assist with feeding. As speech develops, our therapists complete prelinguistic evaluations before surgery to provide early speech assessments. This allows our team to continue assessing after palate surgery and to initiate early intervention if needed. This evaluation is critical throughout childhood to ensure each child has appropriate speech development and articulation. Children also receive the support of our audiologists and otolaryngologists at birth to assess hearing and minimize developmental otitis media and chronic effusions.
Our excellent pediatric dental team includes our orthodontists. Together, they monitor oral hygiene and assist in preparing the child for surgical procedures. Our orthodontists can provide nasoalveolar molding to minimize the width of the cleft and improve the nose in our primary cleft lip infants. They can provide an oral airway prosthesis for some children born with isolated cleft palate and obstructive sleep apnea. This device allows these children to avoid invasive surgery and go home breathing safely, and it is not offered at any other hospital in the state. Later in childhood, our team provides orthodontic preparation for bone grafting and orthognathic surgery.
Cleft lip and/or palate are not always an isolated finding, and our geneticist can evaluate for a potential syndrome and recommend testing if indicated. Families often have questions about the risk of clefting in future children, and our geneticist can also counsel them with risk assessments and education.
It is common for children with clefting and their families to experience emotional, behavioral and academic difficulties at some point. Our team has a dedicated psychologist available who can easily connect our families to assessment, further evaluation and treatment. Some children and their families may need special assistance, and our social worker can help in these cases.
At the end of each visit, each provider meets as a team to develop a comprehensive and coordinated treatment plan. Treatment of a child born with a cleft begins before birth and continues into adulthood. Our success is due to a multidisciplinary team effort and outstanding individualized care for each child.
Head shape clinic
Craniosynostosis, which affects approximately 1 in 2,500 newborns, requires timely and effective surgical intervention to reduce complications and improve outcomes. Studies from the National Institutes of Health suggest a rising prevalence over the past decade, perhaps related to changes in awareness, diagnostic ability, access to care and the fetal environment (maternal diabetes, smoking and constraint-related factors).
While craniosynostosis typically manifests as an abnormal head shape, most abnormal head shapes are not associated with craniosynostosis. The past several decades have simultaneously witnessed an increasing prevalence of deformational plagiocephaly, linked with the Back to Sleep Campaign in 1992, which encouraged healthy infants to sleep supine to reduce sudden infant death syndrome. Recent estimates suggest approximately 50 percent of infants will develop various degrees of deformational plagiocephaly. While craniosynostosis reflects a rarer pathologic condition often necessitating surgical intervention, deformational plagiocephaly does not. So this may make you ask the question: When is an abnormal head shape truly abnormal?
Along with our pediatric neurosurgeons, we have developed the Head Shape Program MDC to comprehensively diagnose and treat patients with head shape concerns. The team includes specialists from:
- Plastic surgery
- Neurosurgery
- Genetics
- Neuroradiology
- Neuropsychology
- Physical therapy
- Cranial orthotics
- Medical photography
The team meets bimonthly to evaluate and treat children with craniosynostosis or moderate-to-severe plagiocephaly. Since its launch in fall 2023, we have also expanded treatment modalities available for children with the most common form of craniosynostosis affecting the sagittal suture. The technique, called spring-mediated cranioplasty, offers perioperative benefits like less invasive strip craniectomy procedures without using a postoperative molding helmet. Additionally, the MDC will begin utilizing 3-D imaging modalities to limit radiation exposure and track aesthetic and functional postsurgical outcomes. We are excited to offer this unique collaborative approach to head shape management for children, families and referring providers throughout the region.
Facial Anomalies Clinic (FACE)
One of the newest MDCs at Children’s Wisconsin is the Facial Anomalies Clinic (FACE). This clinic brings experts together to treat children with complex non-cleft facial deformities, whether soft tissue or skeletal. Aside from clefting deformities, other disease entities affect facial appearance and function and have significant psychological impact. Many of these syndromes appear familial, whether a genetic basis has been identified. Examples include but are not limited to:
- Treacher Collins syndrome
- Goldenhar’s syndrome
- Hemifacial microsomia
- Oculo auriculo vertebral spectrum
- Microtia
- Crouzon syndrome
- Apert syndrome and fibrous dysplasia
Our team includes a geneticist and a genetics counselor, a child psychologist, a craniofacial orthodontist and other representatives from:
- ENT
- Neuroradiology
- Ophthalmology
- Sleep medicine
This clinic’s priority is treating facial skeleton deformities, namely the maxilla and mandible, where complex orthognathic surgical procedures are required. These operations are done in conjunction with the orthodontist both preoperatively and postoperatively to manage occlusal and dental relationships. With the departure of the oral maxillofacial surgery group from Children’s Wisconsin, this clinic fills the void in providing services for children with complex dentoskeletal needs.
Through these three MDCs, plastic surgery provides crucial and unique services for children with complicated craniofacial needs throughout Wisconsin and beyond.

Making miracles come true
How Children’s Wisconsin is making one of the most comprehensive pediatric transplant programs in the United States even more innovative
Many would say it is only appropriate that the first child I had the pleasure of meeting following my hire as the new medical director of Solid Organ Transplant (SOT) at Children’s Wisconsin was named Miracle. While every opportunity to participate in organ transplantation is special, the ability to provide a better life for pediatric recipients and their families is perhaps the most gratifying and, without question, a true miracle. It was a top priority of the dedicated team of physicians, coordinators, administrators and hospital leadership at Children’s Wisconsin to reinvigorate our pediatric kidney transplant program and to reopen our liver transplant program to provide the best possible care to our patients and their families.
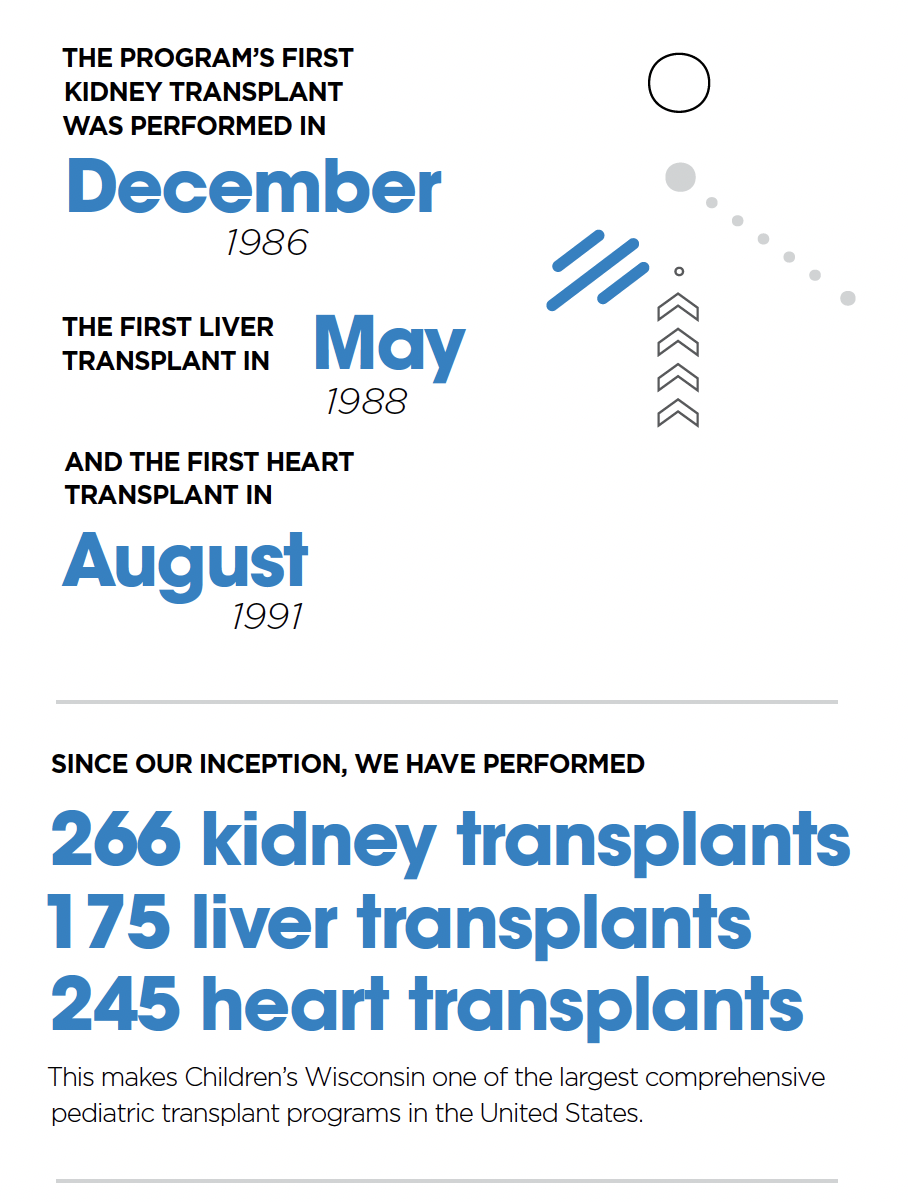
SOT represents a collaboration between Children’s Wisconsin, Froedtert Hospital, the Medical College of Wisconsin and the Versiti Blood Center of Wisconsin. The SOT service line, which includes heart, kidney and liver programs, was the first that transcended the different organizations. The program’s first kidney transplant was performed in December 1986, the first liver transplant in May 1988 and the first heart transplant in August 1991. Since its inception, we have performed 266 kidney transplants, 175 liver transplants and 245 heart transplants, making Children’s Wisconsin one of the largest comprehensive pediatric transplant programs in the United States.
Matthew Cooper, MD, Medical Director of Solid Organ Transplant, Children’s Wisconsin Chief; Professor of Transplant Surgery, Medical College of Wisconsin
Matthew Cooper, MD, Medical Director of Solid Organ Transplant, Children’s Wisconsin Chief; Professor of Transplant Surgery, Medical College of Wisconsin
Expanding under new leadership
Adding to our world-class transplant hepatology and nephrology services, we are excited to welcome new leadership to Children’s Wisconsin. Raj Prasad, MBBS, comes from Leeds, United Kingdom, and is our new director for pediatric liver transplants. Ty Dunn, MD, comes from the University of Pennsylvania and is the new director for pediatric kidney transplants. Both world-class surgeons and esteemed international leaders, Dr. Prasad and Dr. Dunn bring decades of surgical experience in transplants for complex pediatric recipients, living organ donation and hepatobiliary procedures to Children’s Wisconsin. They will be critical in fostering and strengthening relationships with external referring providers, as well as conducting innovative and groundbreaking research.
With our rich history, new leadership and renewed energy, we have sizable aspirations and expectations of the SOT teams. This year alone, the kidney transplant team has completed six deceased donor cases in children ages 4–17, including Miracle. After an almost eight-month hiatus, the liver transplant program has been reactivated, and the first patient was transplanted in September.
We anticipate a robust waiting list for both programs as word of our activities and dedication to providing the highest-quality transplant services makes its way across Milwaukee and beyond. Our heart transplant team, led by Ron Woods, MD, and Steven Kindel, MD, will continue to accept some of the most critically ill patients in the region. All SOT programs share the vision of making Children’s Wisconsin a destination transplant program for patients and families locally and in our region.
Maximizing patient outcomes
Although the deceased donor allocation system rightly prioritizes our patients, the kidney team immediately began investing significant effort and resources toward living donation education and identification, specifically encouraging pairs to consider entrance into the Paired Kidney Exchange (PKE) program. This opportunity allows for an improved eplet-matched donor to maximize patient and allograft survival and immunosuppression minimization known to increase the risk of infections and malignancies, especially over the lifetime of these young recipients. Similarly, our liver transplant team is interested in rapidly reinvigorating our live donor liver program to provide greater access to high-quality allografts and to reduce waiting time.
Making miracles happen with teamwork
Quality and outcomes will remain our guiding light for all SOT programs at Children’s Wisconsin. Recognizing our desire to say “yes” when other transplant programs say “no” means the post-transplant care from our multidisciplinary teams must never be underappreciated. Our efforts to plan, predict and prevent will only take us so far. The expression that transplant is the ultimate team sport is clearly on display at Children’s Wisconsin with the ongoing collaboration of our critical care, radiology, infectious disease and countless consultant teams, as well as our coordinators, nurses, APPs and social workers, who remain the heart and soul of all our transplant programs.
We look forward to the bright future for the SOT programs at Children’s Wisconsin. While some of our faces are new, our commitment and passion have never changed. I know we all feel a sense of pride in our collective efforts to provide these critical services to our children. While we must never forget that every transplant starts with a donor, it’s thrilling to see that every donor can make a miracle come true.
Advancing care for rare and complex bladder exstrophy surgery
How the Multi-Institutional Bladder Exstrophy Consortium facilitates surgical expertise for a rare condition
Bladder exstrophy (BE) is a rare and complex congenital condition with extensive anatomical deformation of the pelvis and genitourinary tract. This occurs in approximately 1 of every 50,000 live births. The critical goals for a child with BE are to preserve kidney function, attain healthy bladder function and continence, reconstruct the natural appearance and function of the external genitalia and achieve milestones that fulfill psychological health. Our goals, however, reach beyond this in the total lifelong care of the BE community.
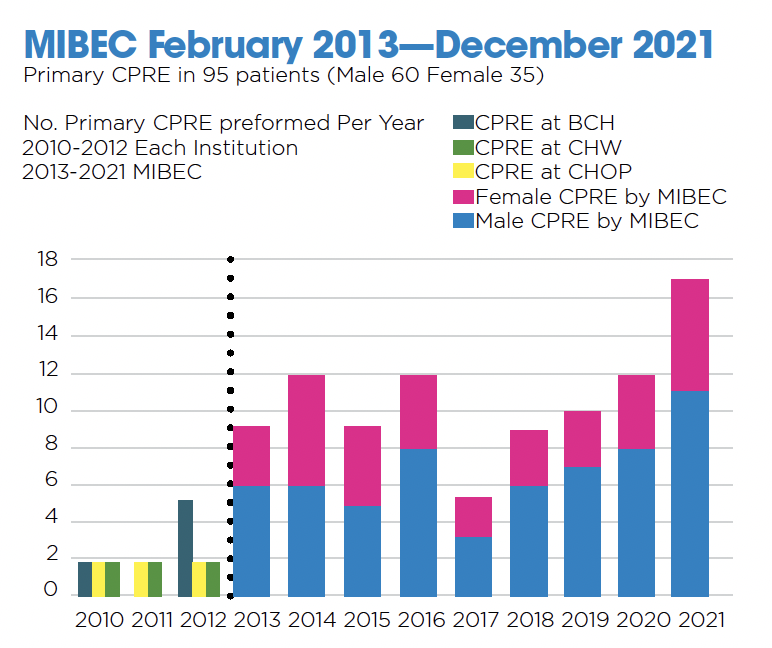
Because BE is rare and complex, many surgeons will see only a few of these children in their careers. Unfortunately, this compromises the ability to develop the necessary surgical expertise. In 2012, we envisioned advancing the care of patients and families with BE. This was the impetus for the Multi-Institutional Bladder Exstrophy Consortium (MIBEC). MIBEC is a novel surgical collaborative focused on refining the single-stage Complete Primary Repair of Exstrophy (CPRE).
Many hospitals treat BE using a planned three-stage surgical approach. However, Michael Mitchell, MD, professor emeritus at the Medical College of Wisconsin, advanced the technique of CPRE — a combination of BE closure, bladder neck reconstruction and epispadias repair in one stage. CPRE is known to be a technically challenging procedure.
From left to right: Douglas Canning, MD; Elizabeth Roth, MD; John Kryger, MD; Michael Mitchell, MD; and Travis Groth, MD
From left to right: Douglas Canning, MD; Elizabeth Roth, MD; John Kryger, MD; Michael Mitchell, MD; and Travis Groth, MD
Establishing the MIBEC
Douglas Canning, MD, and Dr. Mitchell established MIBEC. They founded a small group of surgeons with specific interests and expertise in caring for patients with BE at Children’s Wisconsin, Children’s Hospital of Philadelphia and Boston Children’s.
The MIBEC surgeons at Children’s Wisconsin consist of myself, Travis Groth, MD, and Elizabeth Roth, MD. Our mission is to make meaningful and lasting advancements in caring for children and families with BE. Mentoring or coaching was critical to successfully standardizing the complex surgical technique. We are fortunate to have the expertise of Dr. Mitchell as our coach.
Traveling to each of the three sites for surgery facilitates direct observation, commentary and critique by collaborating surgeons. The collective wisdom and expert coaching by a team of committed expert surgeons is priceless to surgical experience. Video recordings and editing of surgery are used for teaching and future analysis of “game films.”
Refining the one-stage complete primary repair of exstrophy
MIBEC was formed in the fall of 2012, and the first procedure was performed in February 2013. In the first nine years of MIBEC, we performed CPRE surgery for 95 patients with BE. This is well beyond the average experience for most pediatric surgeons.
There have been many benefits of MIBEC. The collaborating surgeons have accumulated a relatively rapid high volume of surgical experience, mastery of the “Mitchell approach” to CPRE, advancement of the surgical technique, detailed outcome analysis, a comprehensive prospective database, scholarly publications, national presentations and teaching videos that promote and share our experience and provide a much better way of teaching the next generation of pediatric surgeons. “The collaboration is a mechanism to learn from each other’s expertise toward promoting the main goal of optimizing care and outcome for rare and complex patients with exstrophy spectrum,” Dr. Mitchell said.
There have been fewer major surgical complications than previously published data. There has not been a urinary tract dehiscence or penile injury. We have not had to perform any bladder augmentations. Several girls, however, had significant urinary retention following CPRE. We were able to use these cases to modify the technique to reduce this issue moving forward. We have also been excited to observe early signs of continence and spontaneous voiding in both boys and girls. It will take years to accurately measure these outcomes, though.
Our surgical philosophy is to anatomically recreate the bladder neck sphincter, which provides resistance to stimulate slow, sustained bladder growth over time. Yet we must keep sphincter pressures low enough to avoid detrimental effects of urinary obstruction and co-existing vesicoureteral reflux — which lead to urinary tract dilation, potential kidney damage and UTIs. Moreover, we strongly believe in strengthening the pelvic floor musculature to augment the sphincter muscles to achieve larger capacities and longer continence intervals. The true benefit of pelvic floor strengthening may not become fully evident until puberty.
Designed for continuous advancement
MIBEC has accelerated surgeon experience and surgical education. Those benefits are also combined with regular meetings for research and clinical outcome analysis. This collaborative model is designed to be transferable to other exstrophy surgeons and other rare, complex surgical procedures. We have been recognized as a Center of Excellence by the Association for the Bladder Exstrophy Community (A-Be-C). We are proud to be the host of the International A-Be-C Conference in the summer of 2024. Follow A-Be-C for more information.
New faculty announcements
Rachel Cambray, MD, is a pediatric anesthesiologist at Children’s Wisconsin and
an assistant professor of Pediatric Anesthesiology at the Medical College of Wisconsin.
Megan Jablonski, MD, is a pediatric anesthesiologist at Children’s Wisconsin and
an assistant professor of Pediatric Anesthesiology at the Medical College of Wisconsin.
Jillian Nard, DO, is a pediatric anesthesiologist at Children’s Wisconsin and an assistant professor of Pediatric Anesthesiology at the Medical College of Wisconsin.
Rushi Patel, MD, is a pediatric anesthesiologist at Children’s Wisconsin and an assistant professor of Pediatric Anesthesiology at the Medical College of Wisconsin.
Adam Striker, MD, FASA, is a pediatric anesthesiologist at Children’s Wisconsin
and a professor of Pediatric Anesthesiology at the Medical College of Wisconsin.
James Yawn, MD, is a pediatric anesthesiologist at Children’s Wisconsin and an assistant professor of Anesthesiology at the Medical College of Wisconsin.
Ahmed Mohamed, DDS, is a pediatric dentist at Children’s Wisconsin.
Caroline Maloney, MD, PhD, is a pediatric surgeon at Children’s Wisconsin and an assistant professor of Pediatric General and Thoracic Surgery at the Medical College of Wisconsin.
Simran Brar, OD, FAAO, is a pediatric optometrist at Children’s Wisconsin and an assistant professor of Pediatric Ophthalmology at the Medical College of Wisconsin.
Samantha Czerniak, OD, is a pediatric optometrist at Children’s Wisconsin and an assistant professor of Pediatric Ophthalmology at the Medical College of Wisconsin.
Aparna Ramasubramanian, MD, is a pediatric ophthalmologist and director of the Retinoblastoma Program at Children’s Wisconsin and an associate professor of Pediatric Ophthalmology at the Medical College of Wisconsin.
Bridget Ellsworth, MD, is a pediatric orthopedic surgeon at Children’s Wisconsin and an assistant professor of Pediatric Orthopedic Surgery at the Medical College of Wisconsin.
Michael Gorelik, MD, is a pediatric otolaryngologist at Children’s Wisconsin and an assistant professor of Pediatric Otolaryngology at the Medical College of Wisconsin.
Matthew Cooper, MD, is the Medical Director of Solid Organ Transplantation at Children’s Wisconsin and chief and professor of Transplant Surgery at the Medical College of Wisconsin.
Ty Dunn, MD, is a solid organ transplant surgeon at Children’s Wisconsin and a professor of Transplant Surgery at the Medical College of Wisconsin.
Kondragunta Rajendra “Raj” Prasad, MBBS, is a liver transplant surgeon at Children’s Wisconsin and professor of Transplant Surgery at the Medical College of Wisconsin.

Advanced practice providers
Anesthesiology, Amy May, APNP
Imaging, Ashley Veale, PAC
Orthopedics, Jerrid Dokey, PAC
Orthopedics, Cynthia Dusel, FNP-C, ONP-C
Orthopedics, Alejandra Poquette, PAC
Otolaryngology, Kathleen Dreyer, APNP
Otolaryngology, Kristin Magner, APNP
2023 new leadership roles and awards
Jonathan S. Ellison, MD
A pediatric urologist at Children’s Wisconsin and vice chair of research for the department of urology and associate professor of pediatric urology at the Medical College of Wisconsin. Dr. Ellison completed the Children’s Hospital Association (CHA) Health Services Research Academy in 2023. The Health Services Research Academy is a hands-on training program that covers every aspect of a professional research project, from conception to publication.
Dr. Ellison was recognized as a Top Reviewer through the Journal of Urology.
Cecille Sulman, MD
Medical director of pediatric otolaryngology at Children’s Wisconsin and professor of pediatric otolaryngology at the Medical College of Wisconsin. Dr. Sulman is president-elect of the Society for the Ear, Nose and Throat Advances for Children (SENTAC) in 2023 and will serve as president in 2024.
David M. Gourlay, MD
David M. Gourlay, MD, is surgeon-in-chief at Children’s Wisconsin and professor of pediatric general and thoracic surgery at the Medical College of Wisconsin. Dr. Gourlay was nominated to the National Surgical Quality Improvement Program Pediatrics (NSQIP-P) Surgical Advisory Committee (SAC) for general surgery in 2023.
John B. Erickson, DO
A pediatric orthopedic surgeon at Children’s Wisconsin and assistant professor of pediatric orthopedic surgery at the Medical College of Wisconsin. The National Board of Osteopathic Medical Examiners (NBOME) and the American Osteopathic Board of Orthopedic Surgery (AOBOS) selected Dr. Erickson as a board item/question reviewer and writer.
Brian T. Craig, MD
A pediatric general and thoracic surgeon at Children’s Wisconsin and assistant professor of pediatric general and thoracic surgery at the Medical College of Wisconsin. Dr. Craig was appointed to the Section on Surgery Publications Committee through the American Academy of Pediatrics (AAP) in 2023.
Valerie A. Flanary, MD, FACS
A pediatric otolaryngologist at Children’s Wisconsin and professor of pediatric otolaryngology at the Medical
College of Wisconsin. Dr. Flanary was the 2023 Vice Presidential Citation Award Recipient for the Triological Society.
Keith Oldham Endowed Chair in Surgery
Dave R. Lal, MD, MPH, holds new position named for former surgeon-in-chief
Dave R. Lal, MD, MPH
Dave R. Lal, MD, MPH
Dave R. Lal, MD, MPH, has been named the first Keith Oldham Endowed Chair in Surgery. This new position was established in honor of Keith Oldham, MD, former surgeon-in-chief at Children’s Wisconsin and former professor and chief of Pediatric General and Thoracic Surgery at the Medical College of Wisconsin. During his 20-year career at Children’s Wisconsin, Dr. Oldham was instrumental in improving the standard of care in pediatric surgery.
Dr. Lal is the medical director of Surgery at Children’s Wisconsin and a professor of Pediatric Surgery at the Medical College of Wisconsin. He first began working with Children’s Wisconsin in 2005, when he was a fellow at the Medical College of Wisconsin. Before that, he earned his medical degree at Creighton University School of Medicine in Omaha, Nebraska. He went on to earn a Master of Public Health from the Johns Hopkins Bloomberg School of Public Health
in Baltimore.
In addition to his extensive training in pediatric surgery, he has completed advanced training in minimally invasive surgery and pediatric cancer surgery. Dr. Lal is committed to caring for every aspect of a child’s surgical needs using state-of-the-art
technology and evidenced-based medicine to provide the highest level of care.
Children’s Wisconsin is proud to be a Surgical Quality Partner of American College of Surgeons. Children’s Wisconsin is an ACS Surgical Quality Partner by participating in select ACS Quality Programs.
2023 Grant Awards
In 2023, Children’s Wisconsin faculty members were awarded grants for a variety of research projects from organizations ranging from our own Children’s Research Network to the National Institutes of Health (NIH) and NASA. The degree of support these programs have garnered is a testament to our faculty’s commitment to research and innovation.

Grants support innovative research programs
Ophthalmology
Elena Semina, PhD, is the Marjorie and Joseph Heil Professor of Ophthalmology & Visual Sciences and a professor of Cell Biology, Neurobiology and Anatomy at the Medical College of Wisconsin. She was awarded the following grants:
- Exploring a new model to study developmental eye diseases — NIH/National Eye Institute
- Identification of Novel Mechanisms Involved in Ocular Phenotypes — Children’s Research Institute (CRI)
- 2023 CRI Program Support: Genetic Studies of Human Development — CRI
- 2023 CRI Fish Facility — CRI
General and thoracic surgery
Brian T. Craig, MD, is a pediatric surgeon at Children’s Wisconsin and assistant professor of General and Thoracic Pediatric Surgery at the Medical College of Wisconsin. He was awarded the following grant:
- Chemokine Responses to Surgery in Neuroblastoma — Clinical & Translational Science Institute (CTSI) of Southeast Wisconsin Mentored Career Development Award
Katherine T. Flynn O’Brien, MD, is a pediatric surgeon at Children’s Wisconsin and assistant professor of Pediatric General and Thoracic Surgery at the Medical College of Wisconsin. She was awarded the following grant:
- Optimizing care for violently injured children and youth: A data-driven and community-based approach to exploring the unmet needs for a multi-disciplinary follow up clinic — CTSI of Southeast Wisconsin Pilot Award
Kirkwood A. Pritchard, PhD, is an investigator at the Children’s Research Institute and professor of Surgery, Pharmacology and Toxicology at the Medical College of Wisconsin. He was awarded the following grant:
- Development of a systems pharmacology agent for treatment of bronchopulmonary dysplasia — NIH Small Business Innovation Research Grant R44
Cardiothoracic surgery
John E. Baker, PhD, is an investigator at the Children’s Research Institute and professor of Cardiothoracic Surgery and Biochemistry at the Medical College of Wisconsin. He was awarded the following grants:
- Determining the impact of space radiation and simulated microgravity on plant root microbial community composition and function — NASA
- Cell Free DNA to assess risk from exposure to medical radiation — CRI
Aoy Tomita-Mitchell, PhD, is an investigator at the Children’s Research Institute at Children’s Wisconsin and professor of Pediatric Cardiothoracic Surgery at the Medical College of Wisconsin. She was awarded the following grants:
- MicroRNA expression patterns in MYH6 tail domain variants in HLHS iPSC-CMs — Medical College of Wisconsin Office of Research Limited Needs Award
- Genetic Etiology of Coronary Heart Disease — CRI
- Mitchell Cord Blood and Tissue Regeneration Program — CRI
- Therapeutic targeting of myosin in the treatment of Hypoplastic Left Heart Syndrome, with Michael E. Mitchell, MD (co-PI) — We Care Fund
Michael E. Mitchell, MD, is the medical director of Cardiothoracic Surgery and surgical director of the Herma Heart Institute at Children’s Wisconsin and professor and chief of Pediatric Cardiothoracic Surgery at the Medical College of Wisconsin. He was awarded the following grant:
- Cell-free MicroRNA in Infant Cardiopulmonary Bypass — Medical College of Wisconsin Office of Research Limited Needs Award
Justinn Tanem, MD, is a pediatric anesthesiologist and critical care physician at Children’s Wisconsin and assistant professor of Pediatric Anesthesiology at the Medical College of Wisconsin. He was awarded the following grant:
- Evaluating the Efficacy of Human Recombinant Dornase Alpha on Cell Free DNA Concentration, with Mitchell Lab, Michael E. Mitchell, MD (co-PI), and Aoy Tomita-Mitchell, PhD (co-PI) — Herma Heart Institute
Children’s Wisconsin
Children’s Wisconsin successfully completed the reverifications from the American College of Surgeons:
- Level I Children’s Surgery Center (the only one in Wisconsin)
- Level I Pediatric Trauma Center
Keeping you informed
Connect with physician liaisons in person or virtually
The Children’s Wisconsin physician liaison team is here for referring physicians whenever and wherever you need us.
In addition to serving as a link between Children’s Wisconsin and referring physicians, your liaisons can:
- Provide information about services and programs offered by Children’s Wisconsin
- Direct you to continuing education opportunities
- Facilitate solutions to referral issues
METRO MILWAUKEE
Lisa Magurany
Manager, Physician Relations
414-266-4743
lmagurany@childrenswi.org
SOUTHEAST WISCONSIN
Margie Berg
414-336-1342
mberg2@childrenswi.org
NORTHEAST WISCONSIN
Diane Dorow
920-370-9381
ddorow@childrenswi.org